HPI
A 25M with an unremarkable PMH presents with 3 days of atraumatic left medial ankle pain, redness, and swelling with no other associated symptoms. He is unable to bear weight or ambulate today due to pain.
Physical exam reveals an erythema and tenderness just posterior to the left medial malleolus with no palpable ankle joint effusion.
Ultrasound
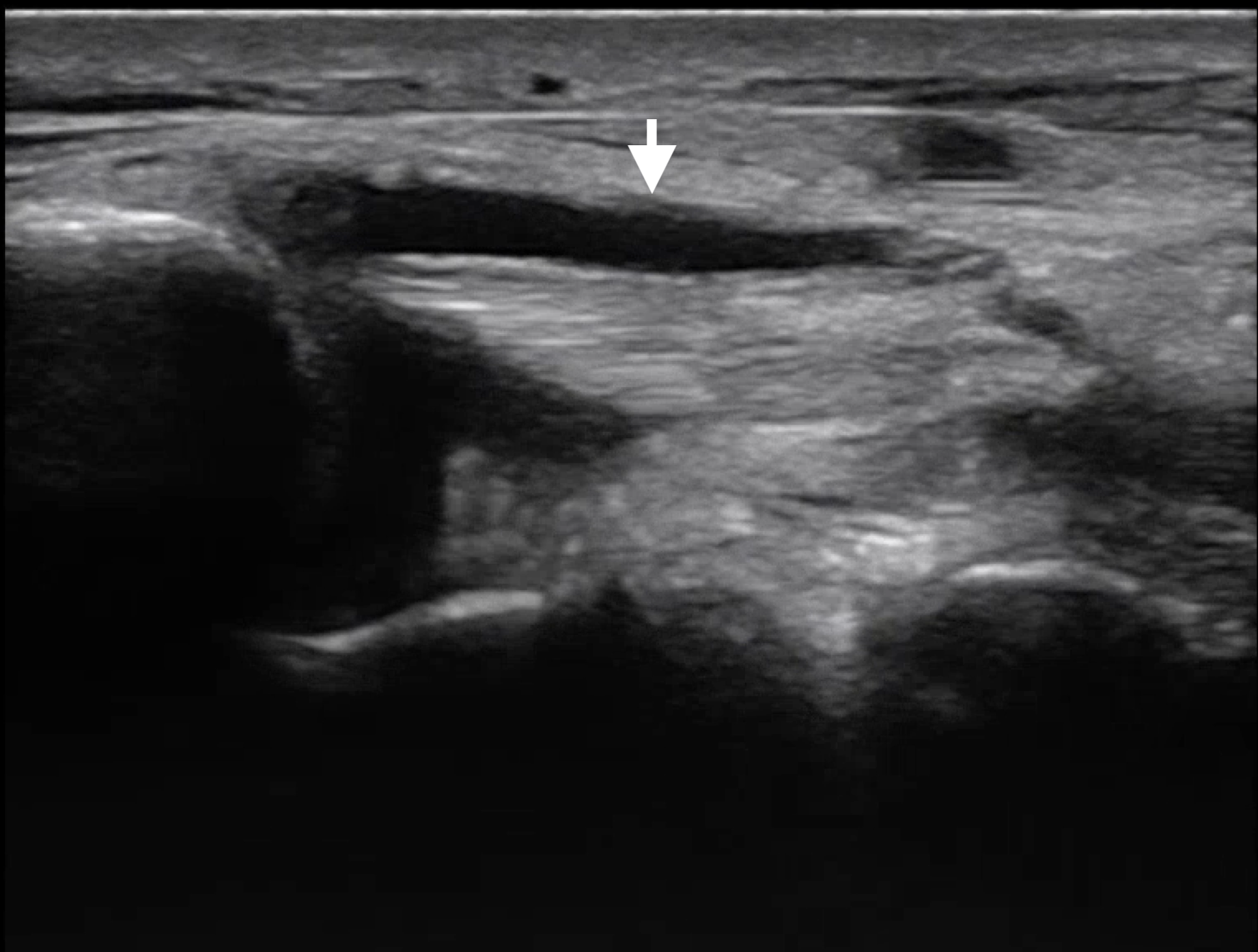
POCUS of the left lower extremity demonstrated no DVT in the femoral or popliteal veins, no abscess in the overlying soft tissue, and no joint effusion in the ankle. Fluid was noted surrounding the posterior tibial tendon, shown below in two planes.
The unaffected contralateral tendon is shown for comparison.
Characteristic findings of tendinitis on ultrasound include hypoechoic areas of inflammation, tendon thickening, or peritendinous fluid. POCUS is also useful to assess for other conditions like tendon rupture or tears.
Case Conclusion
CT imaging showed thickening of the posterior tibial tendon with surrounding edema suggestive of tendinopathy with no evidence of abscess. Antibiotics were started for possible infectious etiology. Patient was ambulatory after pain control and was given a referral for orthopedic followup.
Happy scanning!