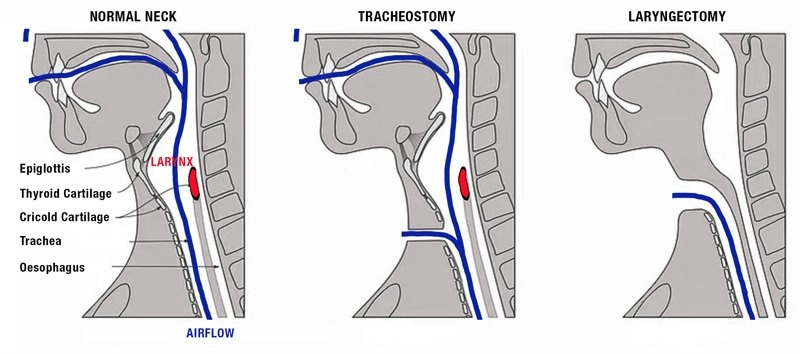
What is the difference between tracheostomy and laryngectomy?
Laryngectomies do not have a connection between the oropharynx and upper airway and cannot be intubated via mouth or nose.
Tracheostomy complications are more common and will be the focus of today's emails. Laryngectomies have become a rarer procedure.
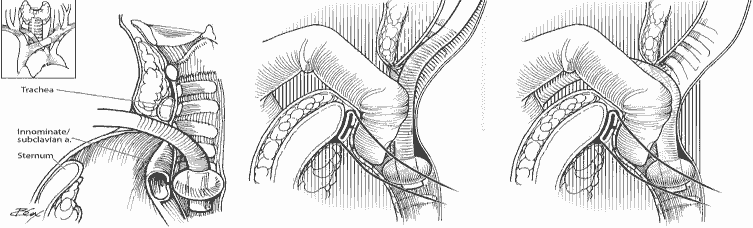
Tracheo-innominate artery fistula
Presentation
Massive hemorrhage from tracheostomy, usually within 3-4 weeks of placement
Workup
CTA, bronchoscopy, local exploration
Note, there is high risk of recurrence so workup should be done even if bleeding has stopped.
Management
Emergent consult to ENT, general surgery, or vascular surgery.
Obtain access, transfuse blood products, reverse anticoagulants.
External compression over sternal notch
Compress innominate artery with overinflated cuff.
If tube is cuffed, overinflate cuff with up to 50ml air to compress innominate artery.
If tube is uncuffed,
If tracheostomy > 7 days, exchange with cuffed tube and overinflate
If tracheostomy < 7 days, exchange under endoscopy or over a bougie if endoscope is not available.
Digital compression of innominate artery (Utley Maneuver)
Insert ET tube via mouth or stoma deep to innominate artery, then insert finger into stoma and digitally compress innominate artery.
Disposition
Low threshold for admission to step-down or ICU setting.
Obstruction
Presentation
Respiratory distress with minimal airflow around tracheostomy, sometimes with clear mucus plugging.
High risk in small tube size.
Workup
Attempt to pass flexible suction catheter.
Can visualize via endoscopy
Management (stop after each step to assess resolution of obstruction)
Oxygen via face mask and via tracheostomy.
Remove external devices (i.e speaking valves, dressings, obturators)
Remove inner cannula
Suction outer cannula with flexible suction
Deflate cuff to allow air flow around tube, assuming tube is obstructed
Remove tracheostomy
BVM via face or stoma. Be sure to occlude the end that you are not ventilating though to prevent air leak.
Reintubate if needed. Orotracheal intubation preferred, but can also intubate via stoma if needed (i.e. upper airway blocked by tumor)
6-0 tube or smaller if intubating via stoma.
Disposition
Discharge with ENT follow-up if obstruction if cleared, stable respiration
Admit to ICU if significant hypoxic event or tenuous airway patency 2/2 recurrent obstruction.
Admit to stepdown/floors otherwise
Decannulation
Presentation
Partial or complete displacement of tracheostomy tube, w/ poor air movement.
Workup
Attempt to pass flexible suction catheter.
Visualize with endoscopy.
Management
High flow oxygen to face and stoma
If tracheostomy < 7 days old, replace only under direct visualization with endoscope. If no endoscopy, then orally intubate.
If tracheostomy > 7 days old, place new tracheostomy tube in stoma. If there is resistance, reattempt with a downsized tube.
Assess for subcutaneous emphysema, which can indicate you are in a false-passage or tracheal injury.
Monitor with capnography
Disposition
Admit if difficult reintubation, requiring downsizing of tube or increased airway secretions
Admit to ICU if pt required orotracheal intubation, significantly increased suction burden, or AMS requiring ICU monitoring.
Discharge with ENT followup if patient had mature tracheostomy with tube replaced easily and placement is confirmed by capnography/bedside endoscopy.
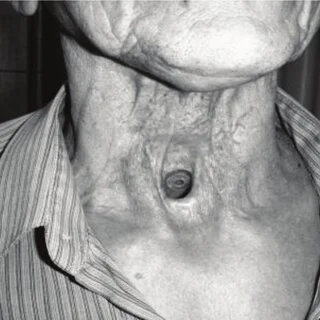
Laryngectomy patients
Less common procedure now
No anatomic connection from trachea to face.
Cannot be nasally or orally intubated.
Nasal cannula or face mask will not deliver gas to lungs.
Some patients may have tracheoesophageal puncture voice prosthesis that can dislodge and become aspirated. You should be able to see this in the stoma.
Workup
CXR, +/- CT chest for foreign bodies, alternate lung pathologies
Consider CT neck w/ contrast, bronchoscopy, cultures for infectious workup
Management
O2 via stoma only. Do not intubate via mouth or nose.
ENT consult for infections, prosthesis aspirations
Disposition
Discharge home if reversible etiology (i.e. obstruction/secretions) that has been resolved without complication. May discharge minor soft tissue infections in consultation w/ ENT
Admit aspirated TEP prosthesis for retrieval and monitoring, or if cause of dyspnea is unclear.
References:
Manning Sara, Bontempo Laura. Complications of Tracheostomies and Laryngectomies. In: Mattu A and Swadron S, ed. CorePendium. Burbank, CA: CorePendium, LLC. https://www.emrap.org/corependium/chapter/reckOdDn9Ljn7sBLy/Complications-of-Tracheostomies#h.5xyzow82ssmf. Updated September 21, 2023. Accessed December 16, 2023.