Epistaxis is one of the most commonly encountered ENT emergencies in the US
Main causes:
Local: Epistaxis digitorum (nose picking), Foreign bodies, Intranasal neoplasm/polyp, Irritants (e.g., cigarette smoke), Medications (e.g., topical steroids), Rhinitis, Septal deviation/perforation, Trauma, Vascular malformations/telangiectasias
Systemic: Hemophilia, Leukemia, Medications , Conditions causing platelet dysfunction , Thrombocytopenia
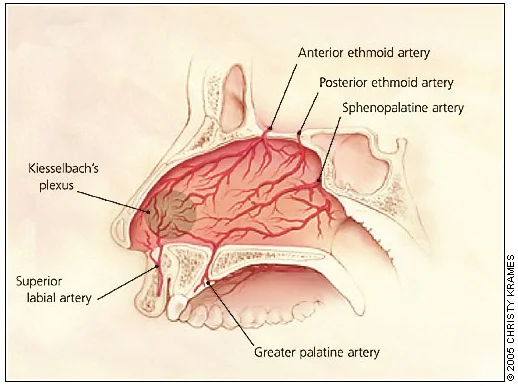
Anatomy:
The vascular supply - from branches of the internal carotid arteries and branches of the external carotid arteries
The anterior portion of the nasal septum - Kiesselbach’s plexus - majority of epistaxis
Posterior epistaxis - mainly sphenopalatine artery and terminal branches of the maxillary artery
Where do you start with nosebleeders?
Assessment:
The usual: ABCs? Is your pt tolerating his/her secretions? Vitals? => Have the pt lean forward applying direct pressure on bilateral nares for at least 10 min, now we can ask some questions.
History:
Onset, duration, and laterality of the current bleed?
Frequency, associated factors?
Review of systems: skin rashes (petechiae/pupura), easy bruising
Previous medical history: hepatic disease (cirrhosis), renal disease (uremia), nasopharyngeal carcinoma
Social history: smoking (irritant), recreational drug use (specifically cocaine and other inhalants)
Medication review: NSAIDs, aspirin, ADP receptor blockers, anticoagulants
Family history: coagulation disorders
Management: the bleeding does not stop after direct pressure. What’s next?
=> have the pt blow her nose to get rid of the clotts, examine the nares, look at the posterior oropharynx, if seems like an anterior nosebleed use topical vasoconstrictors (oxymetazoline and LET), cocaine and topical hemostatics like TXA soaked pledget
=> if patient continues to bleed, look for the source and attempt to cauterize chemically with silver nitrate or electrically. Although that may not work on active bleeding
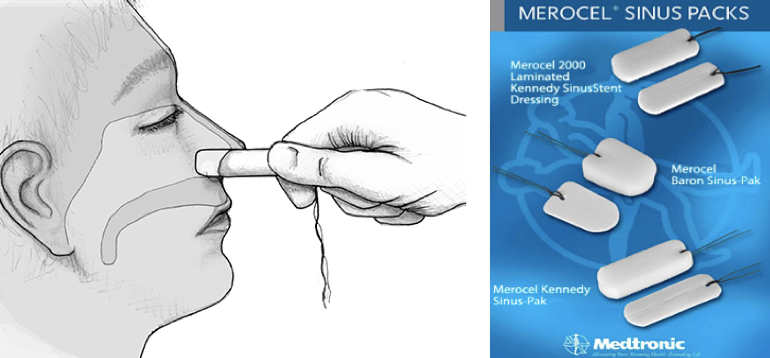
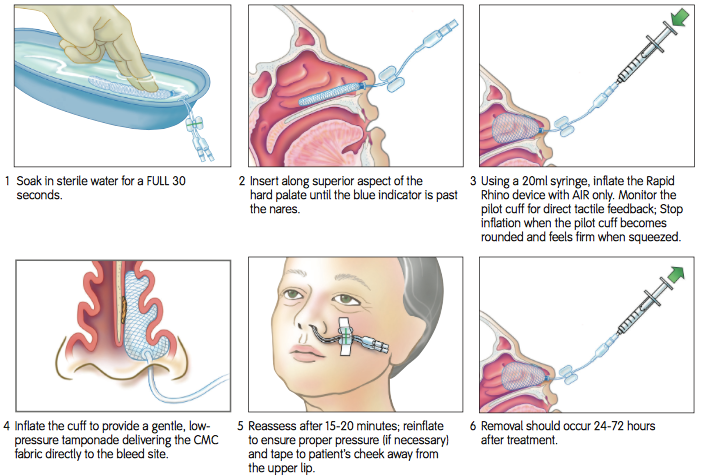
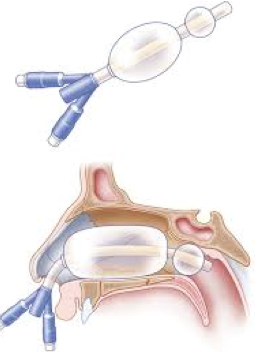
=> if that did not work next step is nasal packing with nasal tampons, Rhino Rocket or balloon devices
Nasal tampon:
Rhino Rocket:
What if the bleeding doesn’t stop?
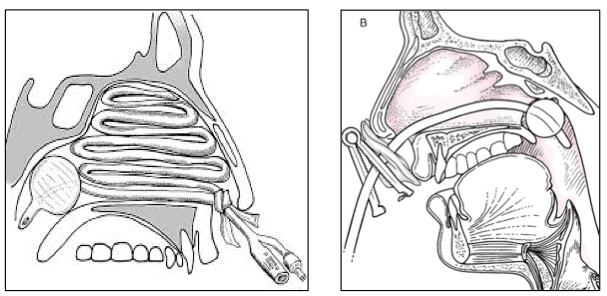
It's most likely a posterior bleed and now you should be sweating…
Call ENT/OMFS/IR/in some places Surgery
Get labs
Consider Posterior nose packing: foley that should be available at every institution or specialized devises like Storz.
Consider antibiotics Antibiotics:
First Line: PO cephalexin 250–500 mg QID or PO amoxicillin/clavulanate 250–500 mg TID
Second line: PO clindamycin 150–300 mg QID or PO trimethoprim/sulfamethoxazole DS
Therapy should be continued for 7-10 days.
Foley Catheter in Posterior Epistaxis
Storz
Resources:
The Emergency Department Management of Posterior Epistaxis
http://www.emdocs.net/emergency-department-management-posterior-epistaxis/
EMCrit C3 Epistaxis