You diagnose a patient with cellulitis and you reach the old, familiar mental roadblock: which antibiotic do I use? Sure, you treated your last cellulitis patient with Keflex, but this patient has a small, mild abscess — do we use a different antibiotic?
UptoDate is tedious, and you’ve called the ED pharmacy 15 billion times today already for other med recommendations. Is there a better way?
B E H O L D : The IDSA Practice Guidelines
https://www.idsociety.org/practiceguidelines#/name_na_str/ASC/0/+/
From treating cellulitis to combat-related infections to leishmaniasis, the IDSA has the most current recommendations for you, the practitioner.
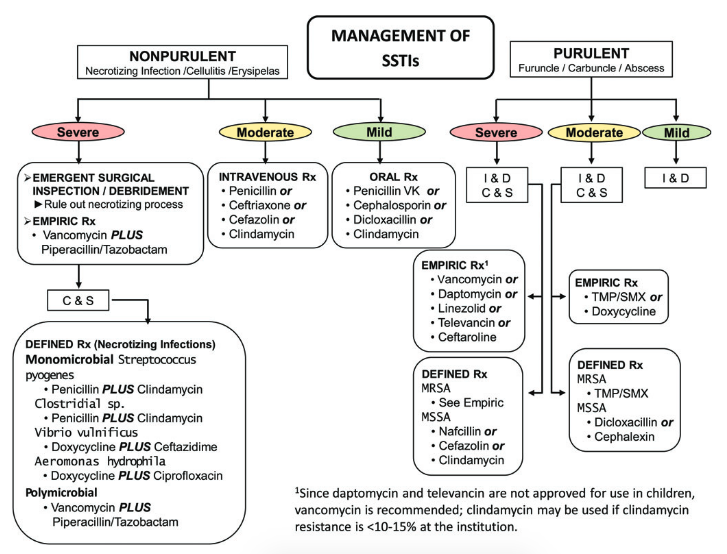
Back to our patient's skin infection. A quick search will yield this handy chart:
Our patient is young, with no comorbidities, and he has a mild, superficial, purulent infection with no systemic symptoms. According to this chart, we could treat with I & D and NO ANTIBIOTICS AT ALL. However, the same patient with a more deep-seated infection, systemic symptoms, or any risk factors would warrant empiric treatment with doxy or bactrim.
IN SUM: The IDSA practice guidelines exist. Use them.