HPI
A 40-year-old female with a PMH of polycystic kidney disease, HLD, and HTN presents with 1 month of episodic dizziness. She was referred to the ED by her cardiologist for an abnormal EKG, and had previously been told that she had an enlarged heart.
Her vital signs are unremarkable. Physical exam is notable for a harsh, blowing systolic murmur. Chest X-ray shows cardiomegaly.
Ultrasound Findings
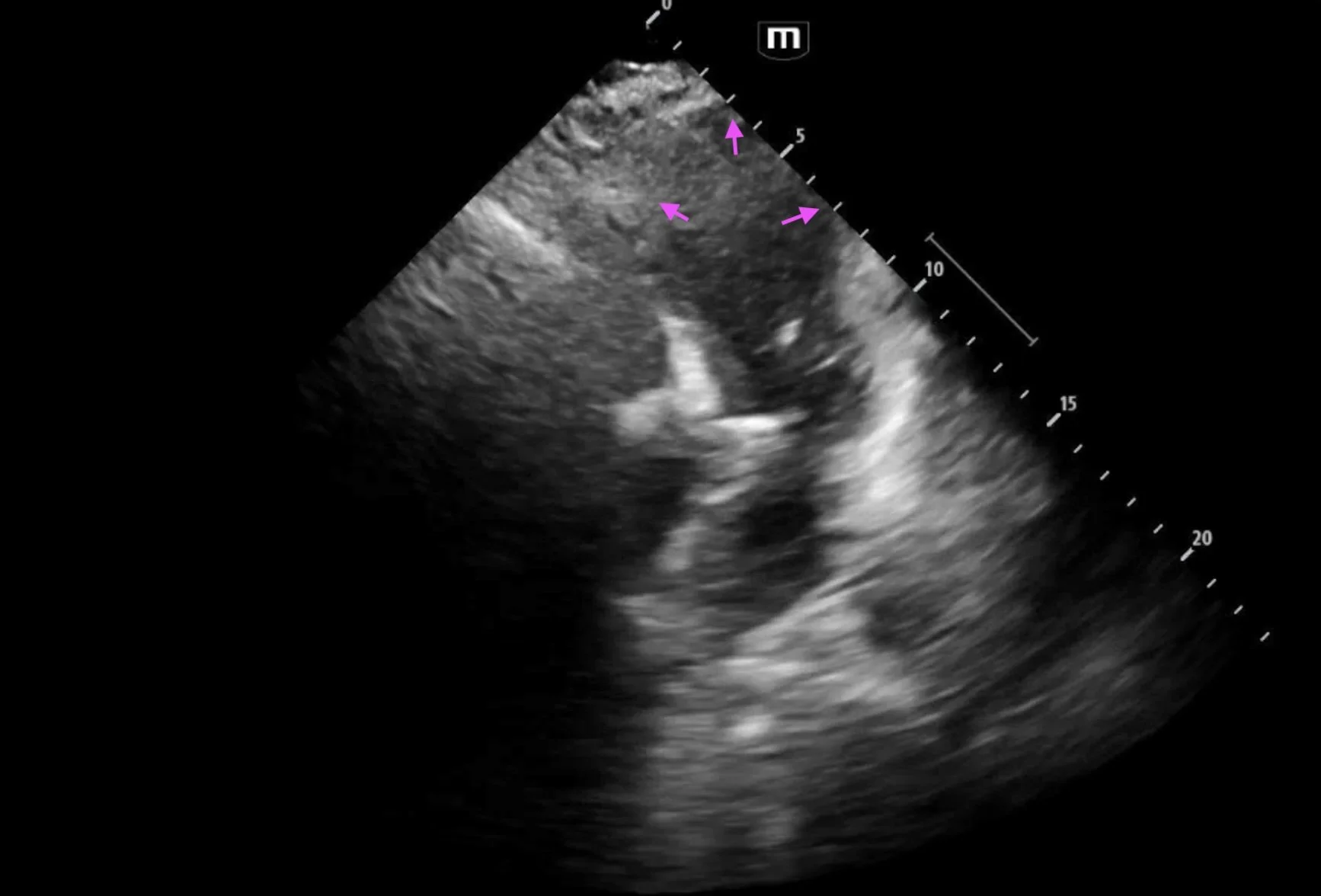
Point-of-care echocardiogram showed no pericardial effusion and was notable for septal thickening to 2.2 cm, concerning for hypertrophic obstructive cardiomyopathy (HOCM).
Echocardiography is the first-line imaging modality for the diagnosis of hypertrophic cardiomyopathy.
Key findings are wall thickening and intraventricular obstruction.
Wall thickening > 15 mm (or > 13 mm in patients with relatives diagnosed with HOCM). This can be measured in the parasternal long or short axis views.
Interventricular septum to posterior wall thickness ratio of > 1.3 in normotensive patients or > 1.5 in patients with HTN
Thickening usually occurs on a focal region of the LV wall
Other associated findings include mitral valve abnormalities, systolic dysfunction, and diastolic dysfunction.
Systolic anterior motion of the mitral valve may occur in HOCM due to the Venturi effect. Septal hypertrophy narrows the LVOT, accelerating blood flow and creating a suction force that pulls the mitral valve leaflet into the LVOT. This causes outflow obstruction as well as mitral regurgitation.
Case Conclusion
Based on these findings, the patient was placed in observation for cardiology evaluation.
Comprehensive echocardiogram revealed findings consistent with HOCM, including severe asymmetric left ventricular hypertrophy, hyperdynamic LV systolic function (LVEF 76-80%), moderate (grade 2) LV diastolic dysfunction, LV outflow tract obstruction, moderate systolic anterior motion of the anterior leaflet of the mitral valve, and moderate mitral valve regurgitation.
The patient was newly diagnosed with and educated about HOCM. She was discharged with metoprolol 25 mg daily and is anticipated to undergo further treatment with mavacamten and possible septal reduction surgery.
References & Further Reading
Happy scanning!