
Here is a light visual sampling of eye pathology.
Pterygium: no acute intervention, follow up pmd +/- opthomology, if impinging on pupil patient will require surgical removal of this benign growth.

Teardop pupil: indicates globe rupture and intraocular foreign body until proven otherwise, protect globe from any external pressure with eye shield, reduce and prevent IOP elevation- elevate head of bed 30 degrees, analgesia, control hypertension, no valsalva maneuvers, prevent vomiting, EMERGENT optho OR

Hordeolum/Chalazion: no acute intervention, warm packs, no antibiotics indicated, pcp follow up
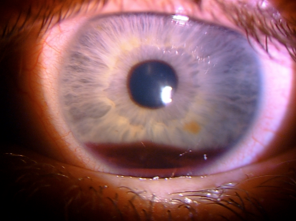
Hyphema: blood in the anterior chamber can be traumatic or spontaneous only needs urgent ophthalmology follow up if up to the pupil. no ED intervention unless signs of intraocular infection then this is an emergency.
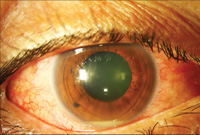
Hypopyon: sign of wide range pathology, can be secondary to trauma, perform woods lamp exam for ulceration, slit lamp exam look for uveitis, urgent opthomology follow up, if infectious etiology suspected systemic antibiotics,
Corneal abrasion: seen on woods lamp exam, raise suspicion for eyelid foreign body be sure to evert both eyelids, flush eye with saline to remove small foreign body, if abrasion is overlying the pupil antibiotic and urgent ophthalmology follow up. patient should not wear contacts on injured eye until healed

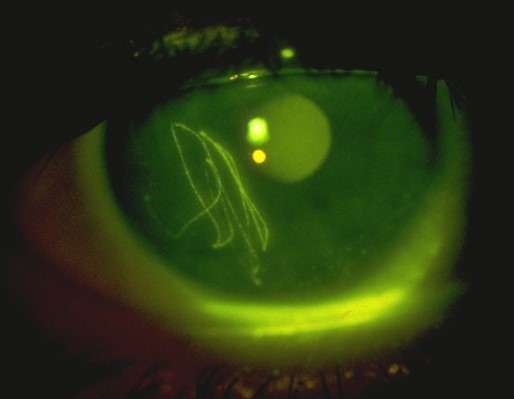
Dedritic ulceration: Herpetic keratitis treat with po acyclovir or opthalmic antiviral, Urgent opthalmology follow up.

Corneal ulceration: ensure no sign perforation-seidel sign, opthalmic antibiotics, urgent optho follow up, if patient wears contacts add coverage for Pseudomonas, do not wear contacts until healed.

Seidel sign: vitreous flowing from site of globe perforation, emergent optho consult in the ER. protect globe from any external pressure with eye shield, reduce and prevent IOP elevation- elevate head of bed 30 degrees, analgesia, control hypertension, no valsalva maneuvers, prevent vomiting,

Exopthalmos: if in setting of trauma with increased intraocular pressure perform lateral canthotomy, suspect retrobulbar hematoma or orbital cellulitis, CT scan emergent optho consult,

Corneal foreign body with rust ring: remove foerign body, urgent follow up for rust ring removal which should be done after 24 hours from initial injury, this is because reepithelialization makes removal easier.
