Dental Trauma
Pulp – inner layer with neurovascular supply
Dentin – most of tooth under enamel
Enamel – thin outer layer
Cementum – outer layer of root surface
Crown – visible part of tooth
Root – part not visible covered by cementum
Primary/pediatric teeth – 20 teeth, 8 incisors, 4 canines, 8 molars, central incisors start at 7 months of age, 20 by 3 years of age (named A->T)
Permanent Teeth – 32 permanent teeth (8 incisors, 4 canines, 8 premolars, 12 molars), rerupt at 6-7 yo and all 32 by 13 yo
Fracture – evaluate for tooth mobility, sensitivity, fracture
Ellis class I: fracture of enamel, tooth is painless, superficial fracture, no intervention needed, refer to dentistry
Ellis Class II: dentin fracture, dentin which is has soft golden yellow appearance can be seen, this has higher risk of pulp necrosis/infection, needs f/u with dentistry within 24h, consider dental block for pain relief, CaOH sealant
CaOH paste comes in 2 tubes that need to be mixed then spread over the tooth after it has been dried off (have patient bite down on gauze or soak gauze with epinephrine)
Ellis III: pulp exposure which is a dental emergency, usually very painful unclear neurovascular damage, if pink or bloody discharge at fracture surface, need emergent dental evaluation in ED, high risk of abscess formation
Cover with CaOH, likely will need root canal by dentistry
Subluxation – tooth is mobile but not displaced, conservative management w/ soft diet and dental f/u
Luxation – tooth is partially displaced from socket, need tooth splinting for 2-4 weeks, need emergent dental consult
Intrusion – tooth displaced apically, if deep > 3 mm, needs emergent dentistry for repositioning and stabilization, if < 3mm, needs urgent 24h dental f/u
Consider CTH w/ face for boney fracture, consider CXR for aspiration, XR
Complete Avulsion – loss of entire tooth from socket, dental emergency
1. when did trauma occur – each minute tooth is out reduces viability by 1%, ideally reposition in 15-30 min
2. where is tooth? Aspirated (CXR), swallowed, embedded in oral mucosa, if you have the tooth, touch only the crown, rinse with water and ideally keep the tooth in the socket
Store tooth in saliva (mouth), milk, saline (less ideal)
3. is tooth primary/permanent
primary tooth should not be re-implanted, needs dental f/u
permanent tooth needs emergent dentistry, periodontal ligament cells can die within 60 min the tooth is outside oral cavity, reimplant tooth to preserve periodontal ligament – splint until definitive management
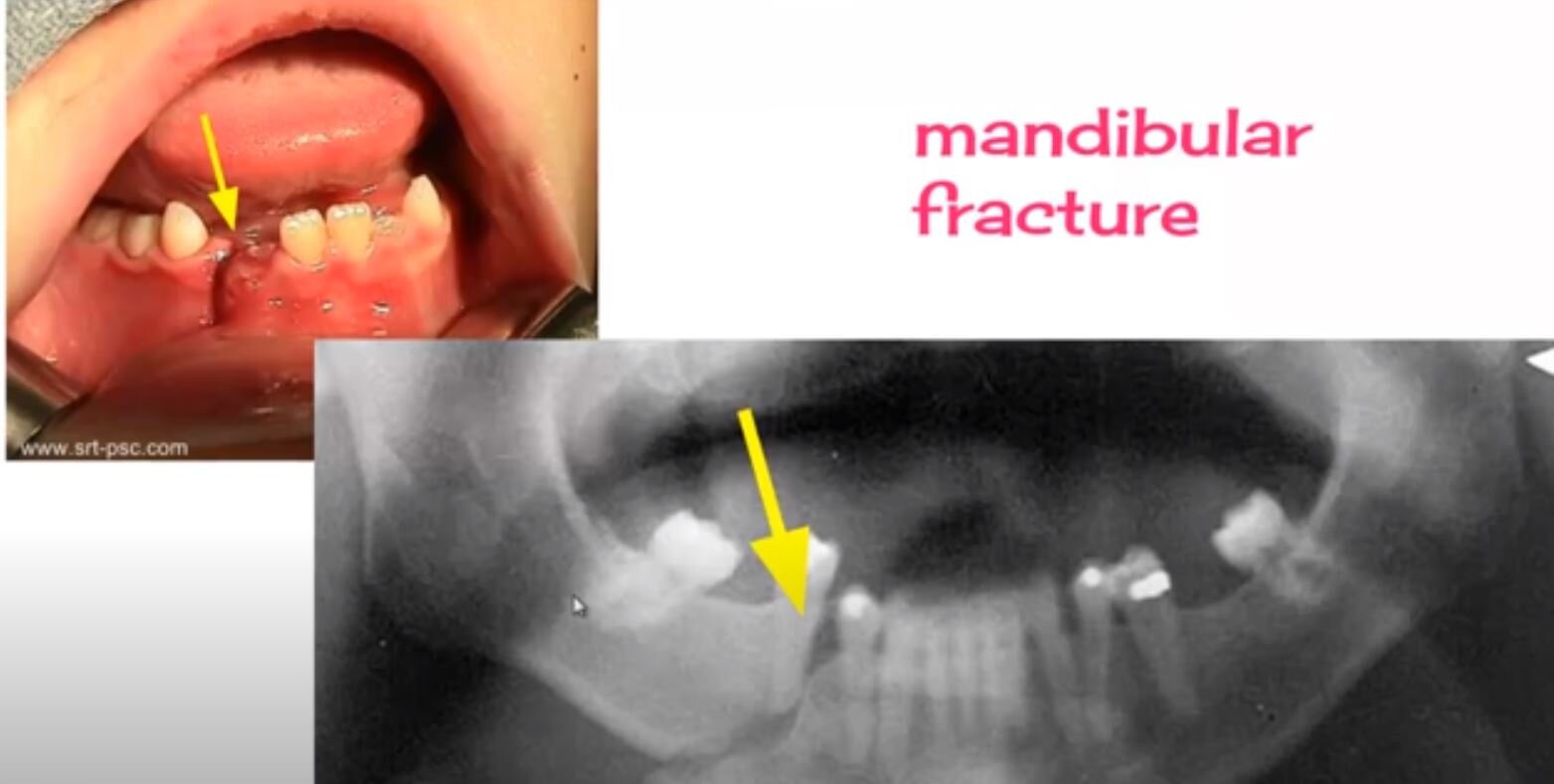
Look for mandibular fracture – can pt open mouth normally, tongue blade test (can pt keep mouth closed to break a tongue blade when twisted), is there pre-auricular tenderness, hematoma at floor of mouth