Case: A 26 yoF who was 5 weeks pregnant presented to the ED after being pushed out of a parked car by her partner. She complained of wrist pain but requested an US to check on her pregnancy. She denied vaginal bleeding or pelvic pain. She had an IUP that was confirmed via US before the assault.
A transvaginal US was performed (video 1) that showed a subchorionic hemorrhage (SCH) > 50% of the gestational sac. Note: be careful not to confuse a large SCH with another gestational sac (image 1).
Image 1
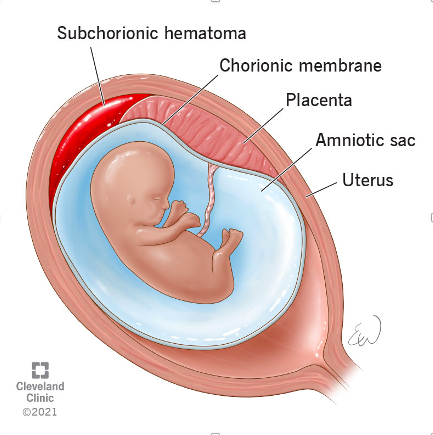
A SCH typically occurs within the first 20 weeks of gestation and is when blood accumulates between the uterine wall and the chorionic membrane (image 2). While many are found incidentally, some patient's may present with vaginal bleeding.
(What is the chorion? It is a membrane that surrounds the developing fetus along with the amnion. It eventually forms the fetal placenta and provides nourishment and protection for the developing embryo.)
On ultrasound, a SCH will typically appear as a crescentic collection with an elevation of the chorion. The echotexture can vary from hyperechoic (acute) to hypoechoic (chronic) based on the duration of the SCH. A SCH is considered large if it is > 50% of the size of the gestational sac. While many resolve during pregnancy, a large SCH can increase the risk of placental abruption, preterm labor, and miscarriage. These patients therefore require close OB follow-up for serial ultrasounds.
Case conclusion: the patient’s workup was negative, she was educated about the found SCH, and given OB follow-up later that week.
Happy scanning!
Ariella Cohen, M.D.
References:
https://radiopaedia.org/articles/subchorionic-haemorrhage-2?lang=us
https://my.clevelandclinic.org/health/symptoms/23511-subchorionic-hematoma