Case 1: A 69 yoF with a PMHx of osteoarthritis presented to the ED with 1 day of worsening knee pain. The workup revealed a moderate-sized effusion and elevated CRP. These factors, combined with her discomfort, prompted the providers to perform an arthrocentesis.
Approach: While there are many approaches you can take to tap a knee effusion, the one I have seen most often is the suprapatellar approach (note: it is best to identify the area with the biggest pocket). Next, gather your equipment for a regular arthrocentesis plus a probe cover. Once you identify your pocket, turn your probe so it is in-plane with your needle. Advance your needle until you see it enter your fluid pocket and aspirate. Remember to put color flow over the expected trajectory of your needle to avoid vasculature.
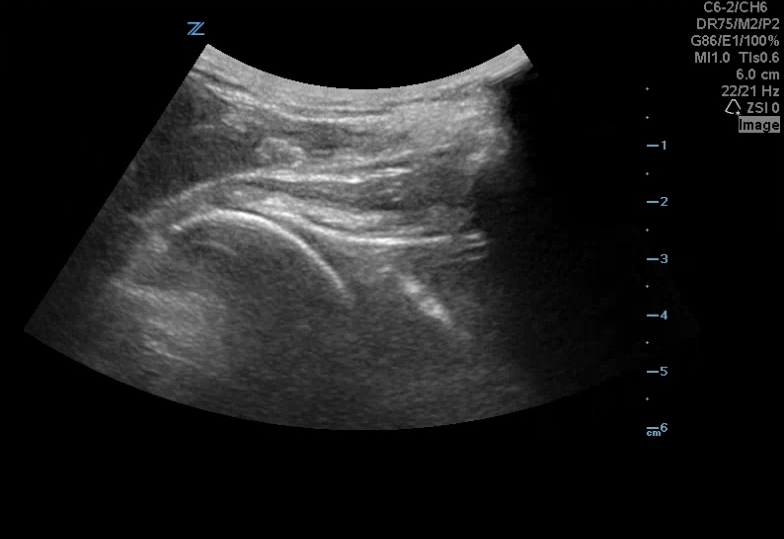
Image 1: Knee arthrocentesis set-up
Video 1 shows the moderate-sized effusion in the suprapatellar region. (note: you can also see a separate, rounded, fluid-filled area, which is the pre-patellar bursae).
Video 2 shows the needle in-plane during active aspiration.
Video 3 shows the needle in the decompressed joint space.
Case 2: A 102 yoF came to the ED with difficulty ambulating due to ankle pain. On exam, she had swelling, tenderness, and pain with passive/active range of motion. Bedside US showed a joint effusion and inflammatory markers were elevated. In conjunction with the family, the decision was made to tap the ankle joint.
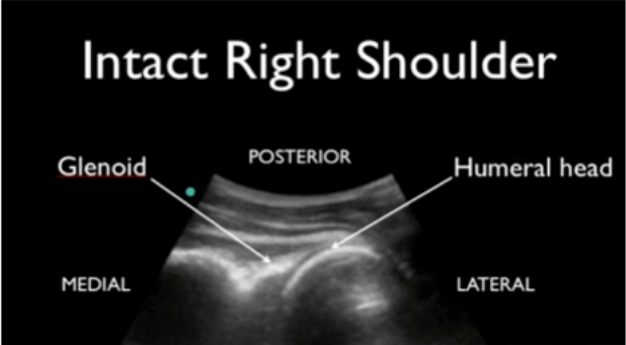
Image 2: normal tibiotalar joint space
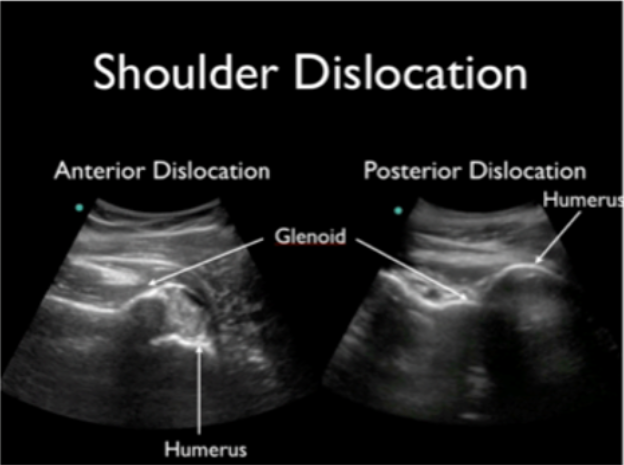
Image 3: tibiotalar joint space with effusion
Video 4 shows a fluid collection at the tibiotalar joint.
Video 5 shows Dr. Tran performing a dynamic aspiration of the ankle effusion.
Results: Results from the arthrocentesis in case 1 showed inflammatory arthritis and case 2 was gout. While neither case turned out to be septic arthritis, both patients felt much better after the tap and were able to ambulate.
Why use ultrasound? Using ultrasound guidance to perform an arthrocentesis allows you to see the exact location of the joint effusion, improving your first-pass success rate. In addition, using color-doppler before the tap decreases the risk of neurovascular injury.
References:
https://coreultrasound.com/knee-aspiration-and-injection/
https://cdn.mdedge.com/files/s3fs-public/Document/June-2017/em049070329.PDF
https://www.tamingthesru.com/blog/mastering-minor-care/ankle-arthrocentesis
Happy scanning!
Ariella Cohen M.D.