This VOTW is brought to you by Drs. Chiu, Butt, Burns, Wong, and Sanghvi on a scan shift.
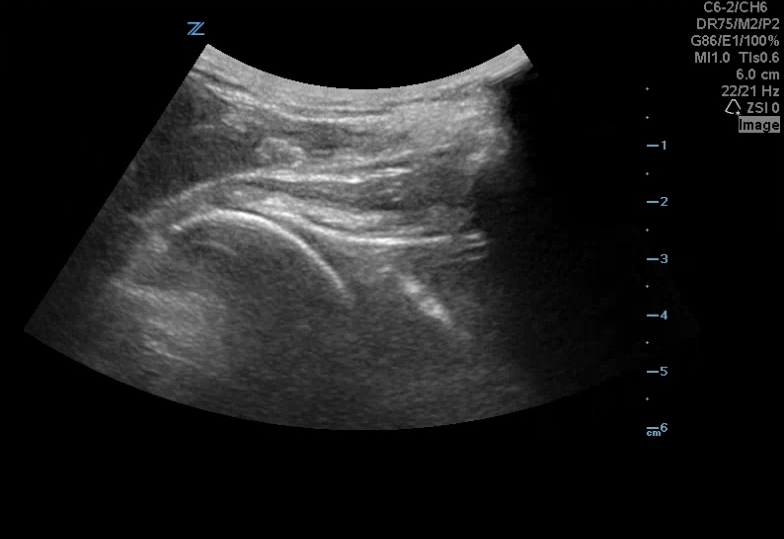
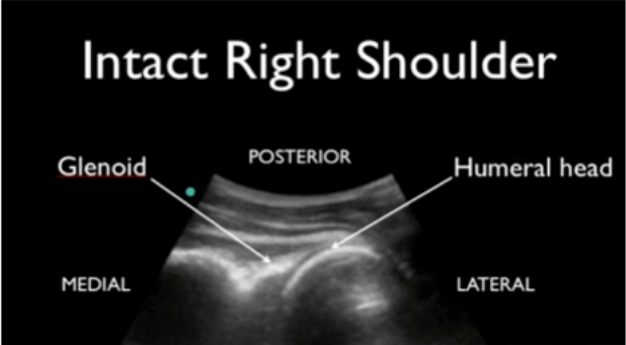
A 42 yoM presented to the ED with a left shoulder dislocation. The ultrasound team looked at his dislocated shoulder (Image 1) and gave an Intraarticular lidocaine injection. The providers reduced his shoulder and then looked for confirmation using ultrasound (Image 2).
How can I do this?
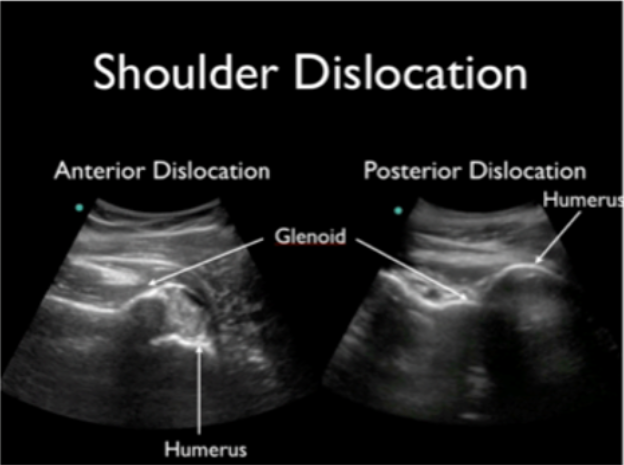
Take your linear or curvilinear probe and place it in transverse orientation on the patient’s back next to the humerus (image 3). The glenoid should articulate directly with the humeral head (image 4). In an anterior shoulder dislocation, the humeral head will be deeper on your screen because it is further from the probe. In a posterior shoulder dislocation, the humeral head will appear more superficial because it is closer to your probe (image 5).
Why use ultrasound?
Ultrasound allows you to check in real-time whether or not the reduction was successful, rather than waiting for x-ray confirmation. I find this particularly useful for my workflow in cases where I am not 100% certain that the shoulder is back in.
References:
Martinoli, C. (2010). Musculoskeletal ultrasound: technical guidelines. Insights into imaging, 1(3), 99.
Jacobson, J. A. (2011). Shoulder US: anatomy, technique, and scanning pitfalls. Radiology, 260(1), 6-16.
5 Minute Sono
The Pocus Atlas
Happy scanning!
Ariella Cohen, M.D.