Diplopia
Case
48F pmh htn, DM presenting with difficulty focusing on distant objects for past few days. Feels like she sees double, all other review of systems normal. On physical exam, pt has a 6th nerve palsy, but has limited R sided rapid alternating movements. CT/MRI/MAR performed shoulder nonhemorrhagic pontine infarct.
Evaluation
1. Is it monocular diplopia or binocular diplopia? -> have patient cover each eye and see if diplopia persists
If diplopia resolves when either eye is covered -> binocular diplopia
If covering one eye resolves the diplopia -> monocular diplopia in the covered eye
Monocular diplopia – refractive error of eye, retinal disease, less common CNS pathology though possible
Usually does not require neuroimaging, can send for optho referral
Binocular diplopia – neuromuscular dysfunction causing misalignment of visual fields, CN palsy, oscular muscle dysfunction, brainstem pathlogy
Usually needs further ED workup for neurologic problem
2. Is diplopia isolated or associated with neurologic signs? Full neuro assessment/exam.
Is there ataxia, vertigo, neuro deficits, dysphagia/dysarthria -> needs rapid neuroimaging and stroke consult to r/o stroke, ideally should have MRI to assess posterior circulation
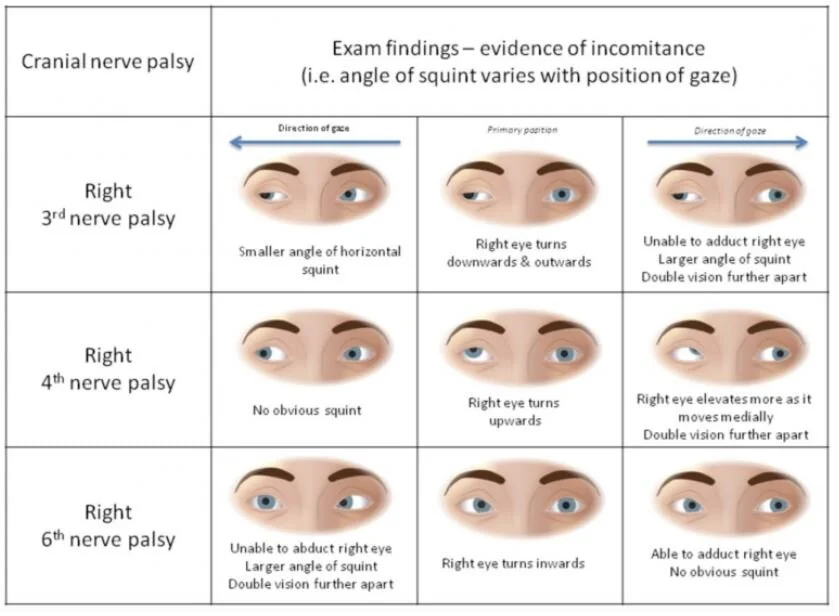
3. Try to localize lesion casing diplopia especially 3rd and 6th nerve palsies by having patient look horizontally and vertically
Isolated nerve palsies are the most common causes of diplopia usually caused by microvascular insult of the extraocular muscles
Isolated 3rd nerve palsy always needs NCHCT and CTA as they are often caused by ischemia or compressive aneurysm
Isolated 4th nerve palsies without other concerning findings can follow with neurology
Isolated 6th nerve palsies usually does not need imaging unless concern for mass/increased ICP, pediatric 6th nerve palsy needs imaging as malignancy is more prevalent than microvascular disease
If there is suspicion of trauma, pt need neuroimaging regardless of whether it’s monocular or not, orbital floor fracture can entrap extraocular muscles or cause a retrobulbar hematoma causing diplopia
Other Diseases to watch for
Cavernous sinus thrombosis – occlusion of cavernous sinus housing CN 3,4,6, often have eye of affected eye, headache, risk factors for thromboembolic disease -> need CT venogram and MRV
Thyroid disease – cause enlargement and fibrosis of extraocular musculature, fatigue, wt loss, TSH/T3/T4
Giant Cell Arteritis - > 50 yo, unilateral HA, ESR/CRP
Myasthenia Gravis – proximal wkns, respiratory distress, fatigable rather than persistent
4. Patients should be dced with neuro/optho f/u as there are many complex motility disorders that need non-emergent MRI or detailed optho exams