This weeks’ VOTW was brought to you by Drs. Hannah Blakely, Patricia Camino, and the ultrasound team that was scanning that day!
HPI: 6 year old female with PMH of atrioventricular canal defect s/p repair, recent strep throat infection presenting for fever x 14 days.
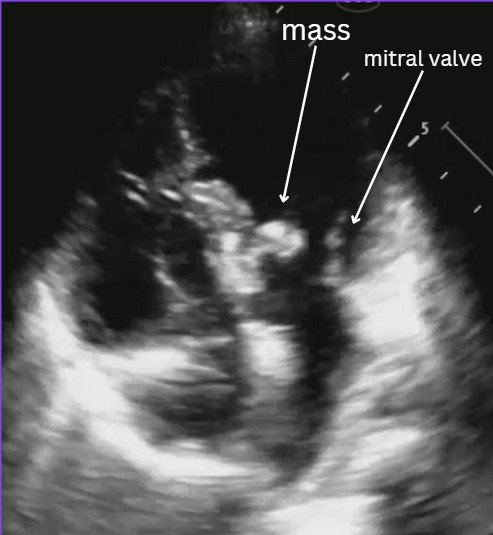
Bedside POCUS showed:
Evaluating for endocarditis on POCUS:
B mode: look for masses, usually on the lower flow side of the valves (ex: mitral valve- endocarditis is more likely to be found on atrial side).
Color flow: you can usually find associated regurgitation of the affected valve
Possible mimics:
Thrombus
Papillary muscle rupture/flail leaflet
Intracardiac tumor
Artifact
Remember that a valve vegetation is one of the major diagnostic criteria for endocarditis. In the right clinical scenario this POCUS finding can highly increase your suspicion for endocarditis.
Case conclusion: CTAP significant for possible splenic and renal infarcts. Patient was admitted for suspected endocarditis. Blood cultures were +MSSA. Pediatric cardiology ECHO was consistent with mitral valve vegetation consistent with endocarditis and septic emboli.
Resources for more info:
Happy scanning!
The US Team