Pacemakers
Or, like, the most complicated things ever
Holy fish-balls, these things are crazy complicated.
Lucky for you all, I have no life – AND DESPITE THIS ENTIRE DOCUMENT ALREADY HAVING BEEN DELETED ONCE – I have (re)gone through a ton of resources to help you, a baller-life-saving-ER-provider, make some sense of these damn things.
We’re going to go over WHY people get pacemakers, WHAT they actually are, HOW they work (barely), and their corresponding EKGs.
If I haven’t thrown my computer out the window, we’ll cover just a couple of pacemaker-malfunction emergencies.
Let’s get started.
CHAPTER 3:
Pacemaker EKGs
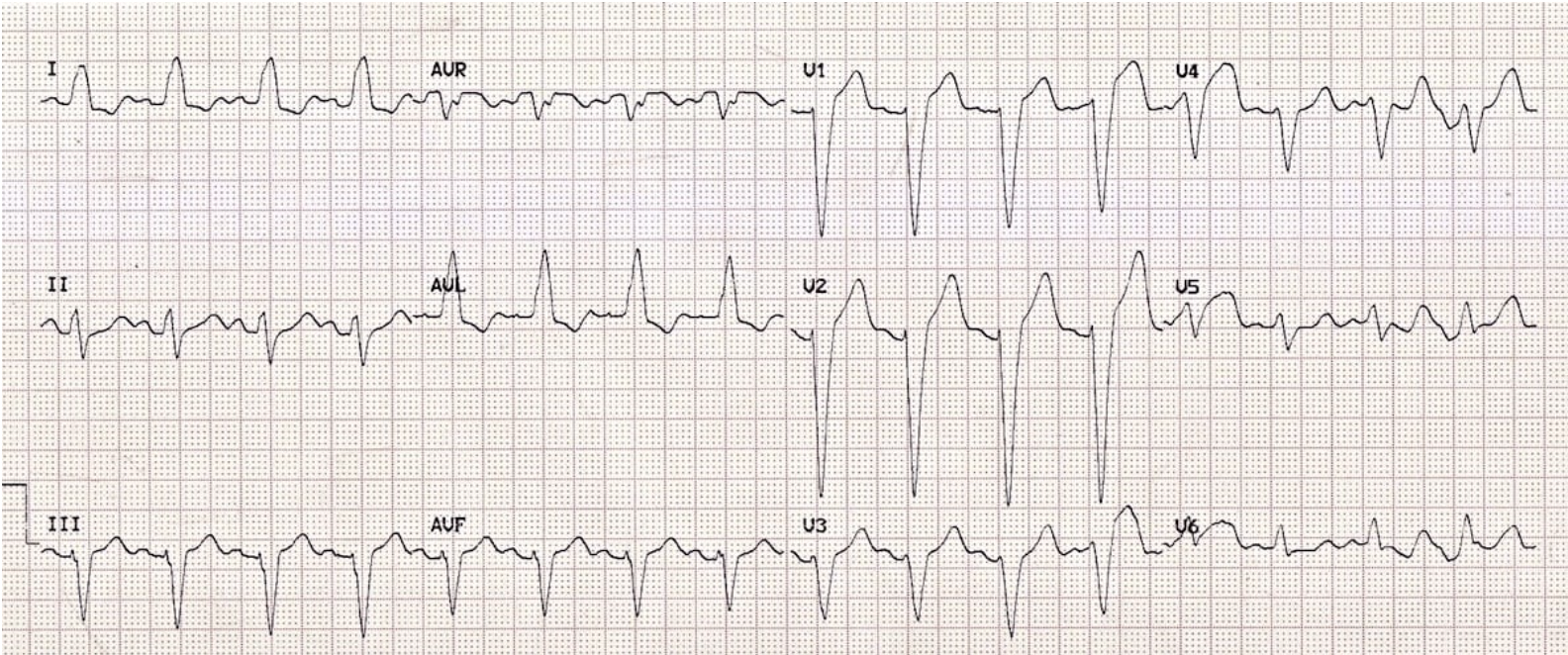
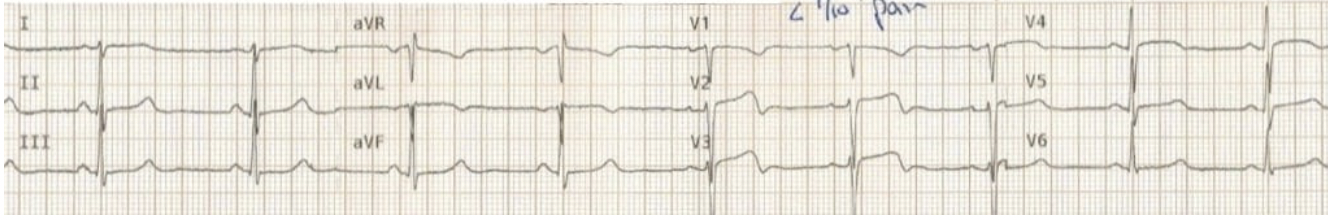
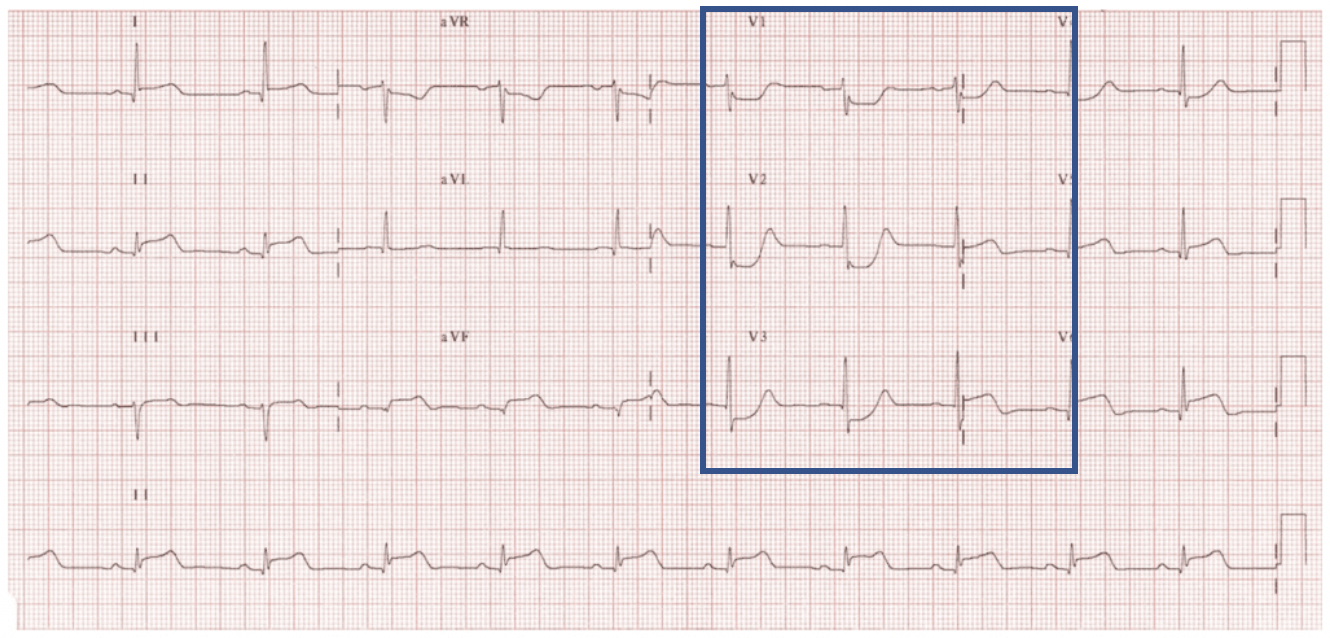
EKG#1 - Atrial Pacing
o Note the tiny lines, or “pacer spikes,” on the EKG that precede P waves
o The pacemaker is triggering atrial beats, depolarizing the atria – the current continues down and appears to depolarize the ventricles through the normal conduction pathway
o This patient may still have a dual chamber pacemaker, but only requires atrial pacing during this EKG
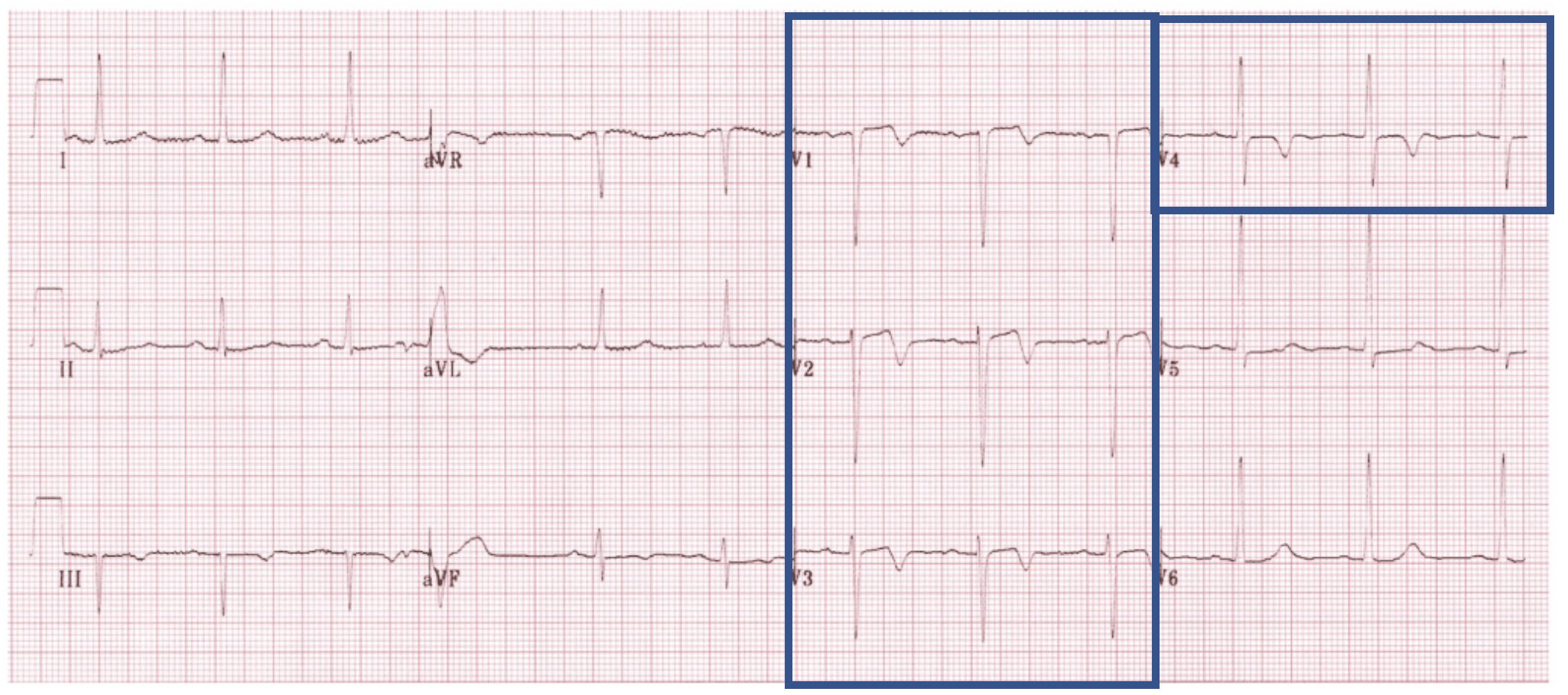
EKG#2 - Ventricular Pacing
o Like we talked about above, the pacing lead is in the RV – the left ventricle relies on the current from the RV, so it looks like a LBBB
o Use modified Sgarbossa, but know that it is not perfect in these patients
EKG#3 - Dual Chamber Pacing
o This patient is having their atria and ventricles triggered by separate impulses
EKG#4 - Bi-Ventricular Pacing
o I’m not going to give you an EKG for this one – in theory you have a RBBB combined with a LBBB, but the patterns are highly variable and non-essential for your knowledge
o Just know you can have two spikes in a QRS… or not…
o If it looks like LBBB, treat it like LBBB
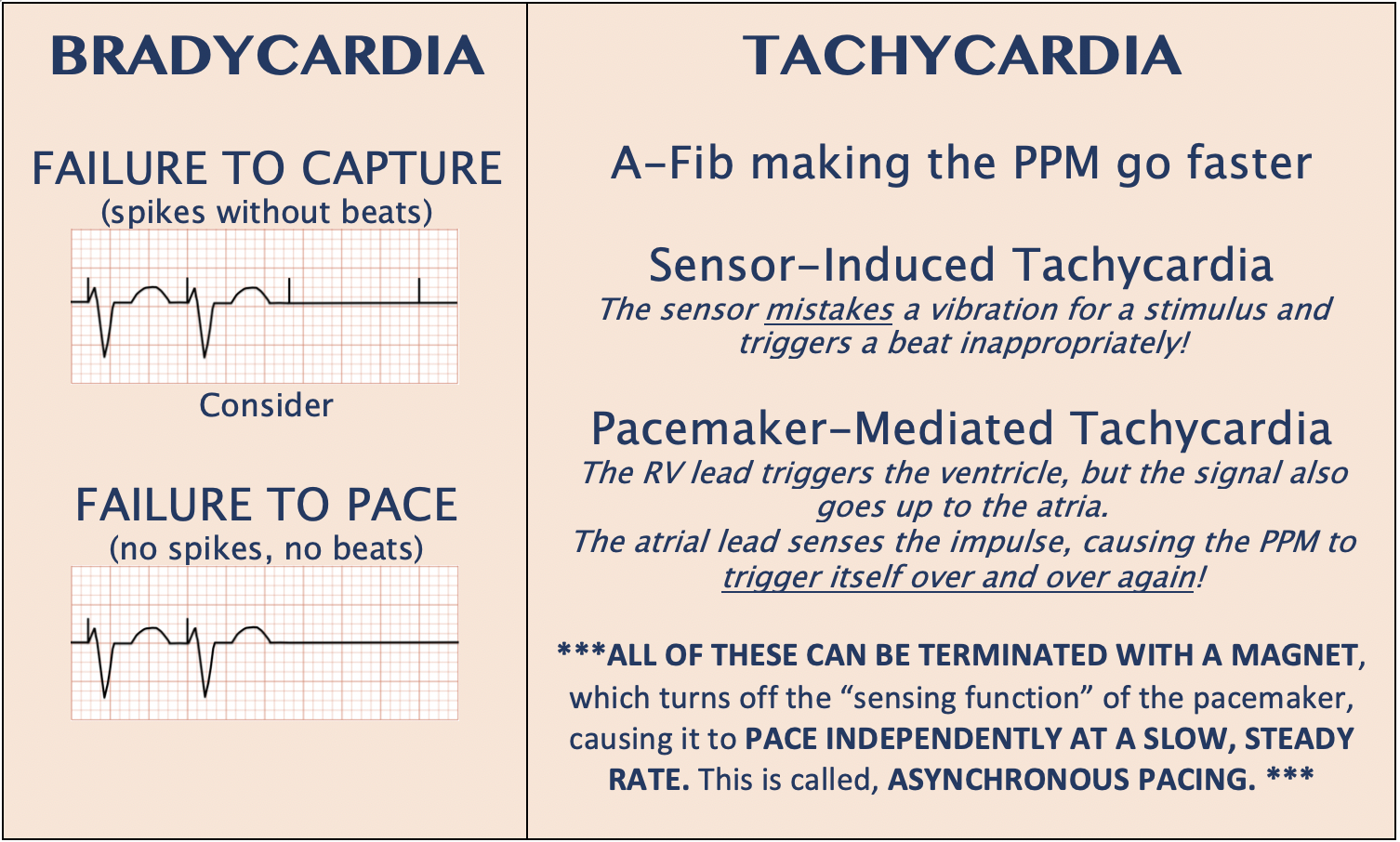
CHAPTER 4:
Pacemaker-Malfunction Emergencies
Lastly, this website has a great algorithm for “ED Approach to Pacemaker ECGs” and the rest of their site is fantastic.
https://canadiem.org/pacemaker-essentials-interpret-pacemaker-ecg/
REFERENCES:
https://litfl.com/pacemaker-rhythms-normal-patterns/
https://johnsonfrancis.org/professional/single-chamber-pacemaker-and-aortic-prosthetic-valve/
https://www.ecgmedicaltraining.com/the-basics-of-paced-rhythms-part-1/
https://canadiem.org/pacemaker-essentials-interpret-pacemaker-ecg/