POTD: Jet Insufflation
Case:
3M with peanut allergy with rash and difficulty breathing. The child was just watching TV when he started itching then developed rash over his entire body and is struggling to breath. Epi pen given but the patient isn’t improving.
PE: severe distress, angioedema in eyes, lips, tongue, stridor and wheezing heard, tachypneic and accessory muscle use, severe urticaria skin
IOs are placed, started on NRB, epi given, Benadryl given, steroids, albuterol administerered
Pt mental status rapidly decreasing becoming cyanotic, BVM attempted but poor air entry, quick attempt at DL shows significant airway edema with no view of the cords…what next
Great 2 min video going over how to perform Needle Cric
https://www.youtube.com/watch?v=vOG08zTZ2YE
Background/Indications
Percutaneous transtracheal jet ventilation is indicated for pediatric patients who cannot be ventilated with BVM or intubated whether due to severe maxillofacial trauma, upper airway bleeding, mass, severe swelling/edema, burns, etc.
Preferred surgical airway for children under 12yo due to small tracheal diameter, prominent hyoid bone which prevents open cricothyrotomy
Not a definitive airway, only a temporizing measure ideally < 30 min until definitive airway is obtained (bronchoscopy, surgical tracheostomy)
Contraindications – significant damage to cricoid cartilage or larynx, if endotracheal intubation is possible
Relative contraindication – complete upper-airway obstruction (surgical cricothyroidotomy preferred
Equipment
O2 source at 10-15L/min
BVM
Large-bore, over the needle IV cath (18 ga+)
Sterile gloves and prep
Depending on what’s available:
3.0 ETT hub (hub is the end of the ETT that connects to the BVM/vent that can be removed)
1 cc syringe + 3.5 ETT Hu
3 cc syringe + 7.5 ETT Hub
Jet Insufflation Kit
1. Ideally, you have time to sterilize the field while the patient is supine
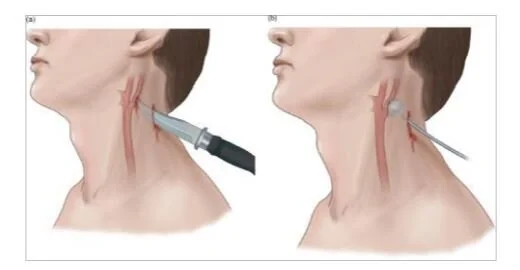
2. Identify the cricothyroid membrane, there are blood vessels sometimes overlying the upper third of the cricothyroid membrane, puncture the lower third if possible
3. Using the largest bore IV, remove the needle portion with the cath
4. twist on a 10 cc syringe (5cc ok) and fill half way with saline
5. stand at the head of the bed and aim the needle caudad at 30-40 degree angle, aspirate as you advance slowly to prevent puncture of the posterior tracheal wall, when you visualize air bubble drawback stop
6. once in the trachea, slide the catheter into the trachea, ideally verify placement in trachea again by aspirating with your 1 cc or 3 cc syringe
7. place either your 3.0 ETT hub directly on the end of the catheter or the 1 cc or 3cc syringe hub combo
8. connect the ETT hub to a BVM
9. suture your catheter in place and plan for definitive airway measures
In our Peds ER, we have a Jet Insufflation kit in the top shelf of the R cabinet in Peds resus. There are three things in the bag: needle, syringe, and tubing. Prep the patient as you normally would.
1. attach saline filled syringe to needle, insert needle same as a standard needle cric while checking for bubble
2. once in trachea, remove syringe and advance the catheter
3. connect the tubing to the end of the catheter, the soft plastic end should be connected to the wall oxygen 10-15L/min
3. Note in the second image, there are holes in the side of the tubing connected to the needle/catheter, these need to be covered for air to go to the patient. You will be controlling the patient’s breathing.
You will be giving breathes at a rate depending on the patient’s age and pathology; the I:E ratio should be usually 1:4 to 1:5
I to E ratio is inspiratory time to expiratory time ratio (same as a vent)
Ex: you want a RR of 20 so each complete breathe is 3s, I:E of 1:5 would be inspiration time of 0.6s with expiration of 2.4s. Of course, in real life, manually trying to time 0.6s inspiration etc is impossible but just try to keep in mind that the time you are giving air should be shorter than the relaxation/exhalation phase. If you ended up giving 1:1 ratio, you might end with a hypercarbic, breath stacked, barotrauma patient.