Dr. Marshall's only request for POTD is that we touch on a trauma topic on the most alliterate day of the week related to trauma. That being.... trauma Tuesday. So here goes....
This guy comes in.
Physical exam is key!!!
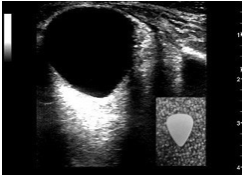
Use your tool. Use POCUS if eye is swollen shut. Tegaderm first, lots of U/S jelly. Is there a pupillary response to light? Is there a consensual response? Is the anterior chamber present? Is the posterior chamber normal appearing (black/round/smooth throughout)? Is there retinal detachment or vitreous hemorrhage? What is the overall shape of the globe? (guitar pick = bad = suspicious for retrobulbar hematoma).
Normal Eye U/S:
Retrobulbar Hematoma on U/S ( measure that pressure and think about clipping that lateral canthus):
Traumatic ocular injuries seen in ED:
Globe rupture
Hyphema
Retrobulbar Hematoma
Lens dislocation
retinal detachment
corneal abrasion/ulceration
Lid Lacerations
Globe Rupture: Prevent increased IOP (elevate HOB, avoid eye manipulation), Seidel test, cover with eye shield, pain meds, topical and systemic antibiotics and Optho consult.
Hyphema: Blood in anterior chamber, Elevate HOB, consult optho, patients at highest risk: sicklers, trauma, bleeding diathesis, the anticoagulated
Retrobulbar Hematoma: Usually 2/2 trauma, can cause optic nerve and retinal ischemia leading to permanent blindness if untreated, A lateral canthotomy is indicated if: proptosis, decreased visual acuity or pain on EOM, afferent pupillary defect or IOP > 40 mmHG
Lens dislocation (aka ectopic lensis): typically 2/2 blunt trauma (less common mechanisms are electrocutions/lightning strike or in Marfan's patients. Painful, + or - lens tremor on exam. Emergent optho consult if elevated IOP.
Retinal Detachment: patient says they see "floaters, black dots and flashes of light." Typically acute painless vision loss. Seen as undulated highly reflective membrane (wavy white line) on U/S. Consult optho.
Corneal Abrasion/Ulceration: fluorescein and woods lamp. Flip eyelid - multiple linear abrasions often imply retained foreign body under eyelid. Antibiotics and analgesia.
Can anyone guess what caused this corneal abrasion?!?!?
(an airbag impact on car accident)
Lid Lacerations: What can we(as ED providers) safely repair in the ED?
Sources:
http://www.emdocs.net/em-in-5-ocular-trauma/
http://www.emdocs.net/core-em-traumatic-ocular-injuries/
http://www.emdocs.net/em-cases-blunt-ocular-trauma/
http://www.emdocs.net/8578-2/
https://emin5.com/2018/04/03/eye-trauma/
https://wikem.org/wiki/Orbital_trauma
https://wikem.org/wiki/Lens_dislocation