So, let's talk about why you went into Emergency Medicine - to talk about rashes, of course! Although you might not always (or rarely?!?) know the exact etiology of the rash, there are some Can't-Miss life threatening rashes that we must be able to recognize in the ED. And rashes account for 5% of all ED visits, so you should be diligent to identify these dangerous diagnoses.
First things first: Describe the rash
Pertinent points on managing rashes:
- STOP IT! Stop the offending agent. Known drugs that induce SJS-TEN include sulfa drugs, penicillin, barbituric acids, aspirins, pyrazolone drugs, and anticonvulsants.
- Rashes can be like a BURN, resulting in abnormal fluid balance, thermoregulation, infection control, and electrolytes. Treat appropriately!
- Treat their PAIN (Make Motov proud!)
- Sepsis management (Make Dickman proud!). If underlying pathology is infectious, treat early and treat appropriately
- Utilize consultants, the sooner the better! Necrotizing infections - surgery. Toxic rashes - Dermatology. ICU and Burn Centers should be on board!
- Steroids??? WAIT - let Dermatology/Burn Center/ICU determine the disease pathology so that steroids will not be given that may cause more harm (SJS/Tens) than good.
There's so much information, but this is just a rough guideline. Remember to rule out life threatening rashes before sending your patient home.
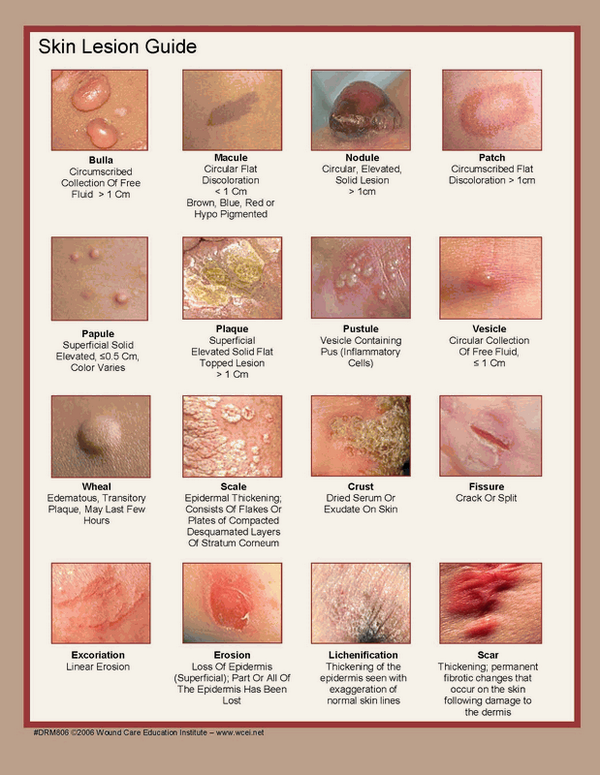
You have to determine the TYPE of rash. The algorithm divides the rashes into 6 types: Maculopapular, Petechial/Purpura, Diffuse Erythematous, Non-erythematous, Vesiculo-bullous, Pustular.
Then branch each type of the 6 rashes into the life threatening etiologies.
Keep in mind that this list is not comprehensive, but a guideline to help identify life threatening rash. If the patient looks ill, be concerned.
Once you identify a life threatening rash, be aggressive and manage appropriately (too many points to address here.) Again, just a guide to look for the DANGEROUS RASHES!. Please see the original reference article attached!
REFERENCES:
https://jetem.org/em_derm_tbl/
http://www.emdocs.net/dont-rash-emergency-physicians-approach-undifferentiated-lesion/