Did you know that over the holidays ER vists across the country >10 fold!

- Laryngotracheal- uncommon but life threatening and often present in distress
- Stridor, wheezes, dyspnea, hoarse voice
- These kids need airway protection and STAT ENT and anesthesia consults!
- Try is airway protection and RIGID BRONCH

- Large bronchi-
- Cough, wheeze, hemoptysis, dyspnea, choking, SOB, decreased breath sounds
- Will also need Rigid Bronch emergently!
- Lower airway- Little distress after the initial episode
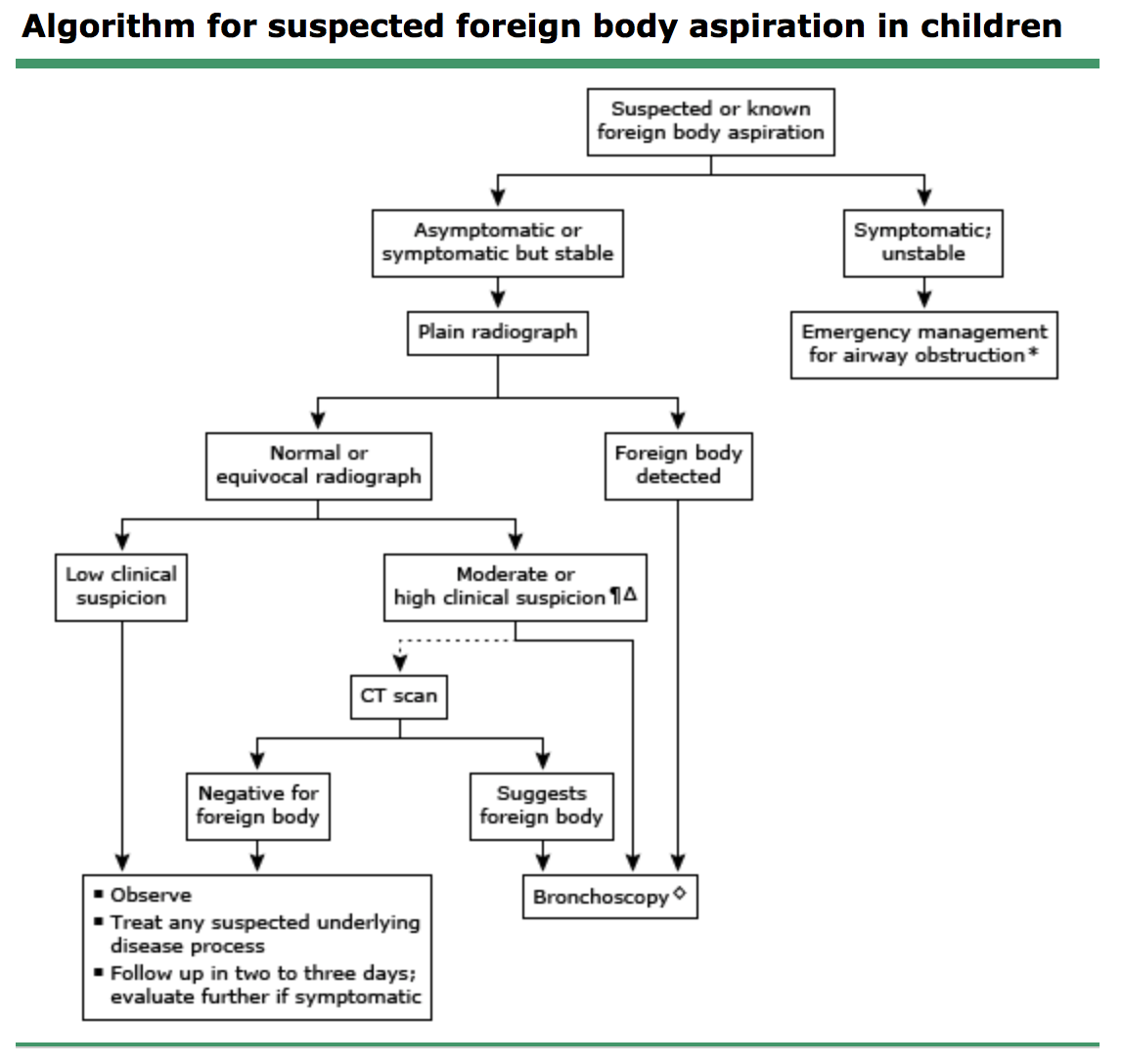
- Xrays should include inspiratory and expiratory films or Left decubitus in younger kids
- If you think its higher up inlay the neck ate PA and lateral views
- Xray findings of lower FB include:
- Hyperinflated lung- lucency distal to obstruction
- Atelectasis
- Mediastinal shift away from the FB
- All children with high suspicion of FBA should be observed and schedule for a bronch
- Rigid> Flexible as it provides better visualization and access for removal of the FB
- Thoracotomy if bronchoscopy is unsuccessful
- Atelectasis
- Pneumonia
- Bronchiectasis
- Abx should be started post procedure







