Epidemiology:
- rare, but high incidence of associated injuries
- mechanism is usually young patients with high energy trauma
Simple vs. Complex:
o simple
- pure dislocation without associated fracture
o complex
- dislocation associated with fracture of acetabulum or proximal femur
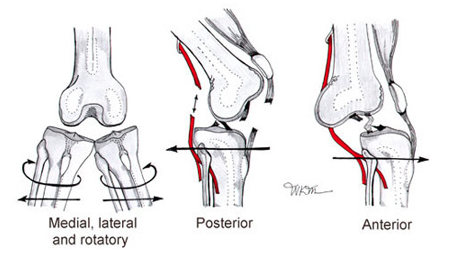
-Anatomic classification:
o posterior dislocation (90%):
- occur with axial load on femur, typically with hip flexed and adducted
- axial load through flexed knee (dashboard injury)
- hip and leg in slight flexion, adduction, and internal rotation
- examine knee for associated injury or instability


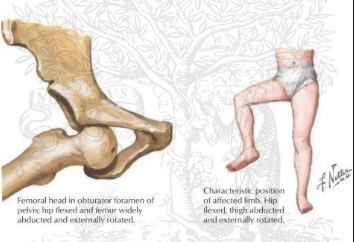
o anterior dislocation:
- associated with femoral head impaction or chondral injury
- occurs with the hip in abduction and external rotation
- hip and leg in flexion, abduction, and external rotation
Imaging:
X-rays:
- Can typically see posterior dislocation on AP pelvis
o femoral head smaller than contralateral side
o Shenton's line broken
o Look at the femoral neck to rule out fracture prior to attempting closed reduction
o AP pelvis after reduction to evaluate associated acetabular fractures
CT:
- post reduction CT must be performed for all traumatic hip dislocations to look for:
o femoral head fractures
o loose bodies
o acetabular fractures
Management:
- Nonoperative
- emergent closed reduction within 6 hours!
- indications:
- acute anterior and posterior dislocations
- contraindications
- ipsilateral displaced or non-displaced femoral neck fracture
- Allis maneuver:
- patient is placed in the supine position
- knee is flexed to relax the hamstring
- assistant stabilizes the pelvis
- longitudinal traction is applied in line w/ axis of femur, and the hip is slightly flexed
- gently adduct& internal rotates the femur to get reduction
https://www.youtube.com/watch?v=2dT1r_U7LQ8
- Captain Morgan technique:
- Position the patient: 90 degrees of hip and knee flexion
- Step one foot up nto the gurney Captain-Morgan style (flamboyant cape optional).
- Position your knee behind the patient’s knee.
- Ideally your foot should be resting on a hard surface like a backboard to allow your foot to push off of it.
- Place one hand (A) under the patient’s knee and the other (B) over the patient’s ankle.
- Use Hand A to lift up on the patient’s femur.
- Plantar-flex your ankle so that your propped knee can lift up on the patient’s femur
- Very gently use Hand B to leverage-down on against the patient’s tibia/fibula.

https://www.youtube.com/watch?v=Uhkc7I4G7ng
- Operative
- open reduction and/or removal of incarcerated fragments
- irreducible dislocation
- radiographic evidence of incarcerated fragment
- delayed presentation
- ORIF
- associated fractures of:
- acetabulum
- femoral head
- femoral neck
Sources: Ortho Bullets, ALiEM, Wheeless’ Textbook of Orthopaedics