Today, we are going to discuss a little bit about thoracic ultrasound in the setting of Trauma: From Core EM (Resident homework) https://coreem.net/core/traumatic-hemothorax/ verbatim:
•Ultrasound (Carmody 2011)
◦High sensitivity and specificity for detecting the presence and quantification of fluid in the pleural space
◦Hemorrhage usually contains echogenic swirling material that moves in response to respiratory movement or the heart beat
◦Best identified using a coronal view of the abdomen (RUQ and LUQ) with a low-frequency probe
◦Twice as accurate as Xray in predicting the volume of a pleural effusion
◦Higher sensitivity for detecting concomitant pneumothorax than CXR
What do we mean by a LOW FREQUENCY PROBE? This is the C-62 which you’re usually using in the FAST exam already. Higher amplitude, lower frequency ultrasound waves can penetrate deeper into the body (as opposed to our higher frequency L83 which has a better resolution but cannot penetrate the way the C62 can).
As stated above, ultrasound is better than CXR predicting volume of a pleural effusion and for detecting a pneumothorax. Let’s look at some pictures!
http://www.erpocketbooks.com/er-ultrasounds/trauma-ultrasounds-from-the-ed/: 
This should be a pretty obvious PTX from radiopedia.org (hint: look at the right ribs and then see if you can follow the air markings all the way up like you can on the left): 
Great picture of the “Bar Code sign” vs “Waves on a beach” for PTX. When you have lung sliding (e.g. NO PTX), the lung slides against the pleura and the moving part creates the sandy “beach” in the picture while the stationary pleura creates what looks like “waves”. Here’s a great link if you want a video and more info! http://rebelem.com/ultrasound-detection-pneumothorax/

Once you’ve established that the patient has a hemo- or pneumothorax that is causing distress, you should place a chest tube. You perform needle decompression IF the blood pressure is unstable and the patient has a TENSION pneumothorax
Here’s a video on how to put in a chest tube: https://www.youtube.com/watch?v=U618Jte_1Uk
More Pearls for Needle Thoracostomy with cheesy music: https://www.youtube.com/watch?v=hiax6H5zUcs

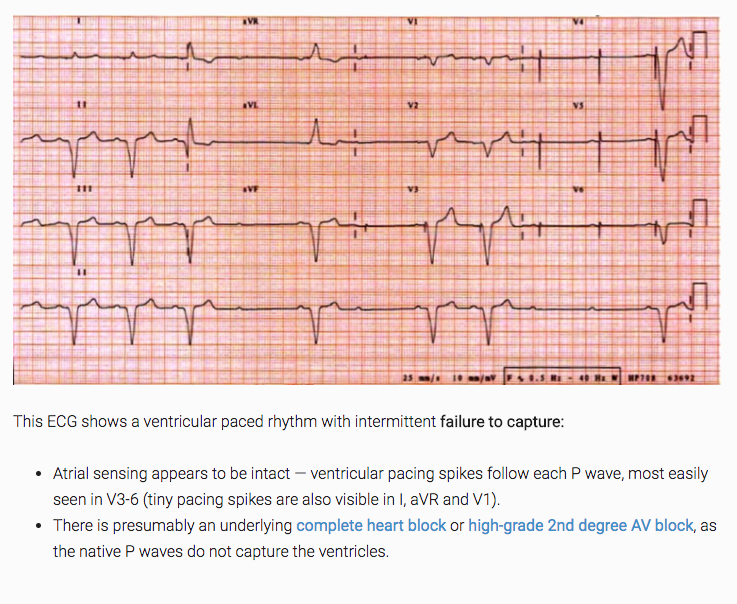 from LITFL!
from LITFL!