Pulmonary Hypertension (PH):
Pulmonary hypertension (PH) is present when mean pulmonary artery pressure exceeds 25 mm Hg at rest or 30 mm Hg with exercise (Normal PA systolic pressures range from 10-30)
Definitive diagnosis via right heart catheterization, rare cause of SOB
In general, there is no cure besides supportive care and treating the precipitant, high rate of mortality
Pathophysiology:
Pulmonary vasculature is meant to be a high-flow, low-resistance circuit.
Cardiac causes
LA or LV disease => ↑ LA pressure => ↑ pulmonary venous pressure => ↑ pulmonary artery pressure => ↑pulmonary vascular resistance
L to right shunt will also cause high pulmonary vascular pressure
Respiratory causes
hypoxic vasoconstriction -> PH
Which leads to => vasoconstriction => altered vascular endothelium and smooth muscle function
=> cellular remodelling => increased vascular contractility => lack of relaxation in response to various endogenous vasodilators => fibrosis of vascular tissue
Symptoms:
Dyspnea (with rest or with exertion), Fatigue, Chest Pain, Syncope, Exertional lightheadedness
Patients with severe pulmonary HTN can develop signs of R heart failure (JVD, hepatomegaly, ascites, edema)
Five types of PH:
Group 1: Pulmonary arterial HTN
Idiopathic
Genetic/Heritable abnormalities
Drug/Toxin induced
Associated with known risk factors (HIV, liver disease, collagen vascular disorders)
Group 2: Pulmonary venous HTN (left heart disease)
Systolic or diastolic dysfunction
Mitral or aortic valve disease
Group 3: Chronic hypoxemic lung disease
Obstructive lung disorders (COPD)
Interstitial Lung Disease
Idiopathic Pulmonary Fibrosis
Sleep-Disordered breathing (OSA)
Group 4: Embolic disease (PE)
Group 5: Miscellaneous
The Workup
EKG:
Most common abnormality is right axis deviation
Signs of R heart strain: S1Q3T3, right atrial enlargement in the inferior leads, incomplete/complete RBBB
Labs:
CBC, CMP often nonspecific
BNP often elevated and correlates with outcomes
Elevations in troponin are associated with higher morbidity and mortality
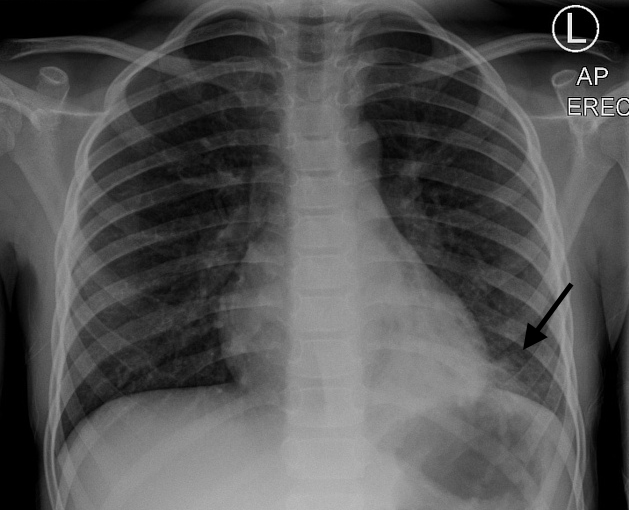
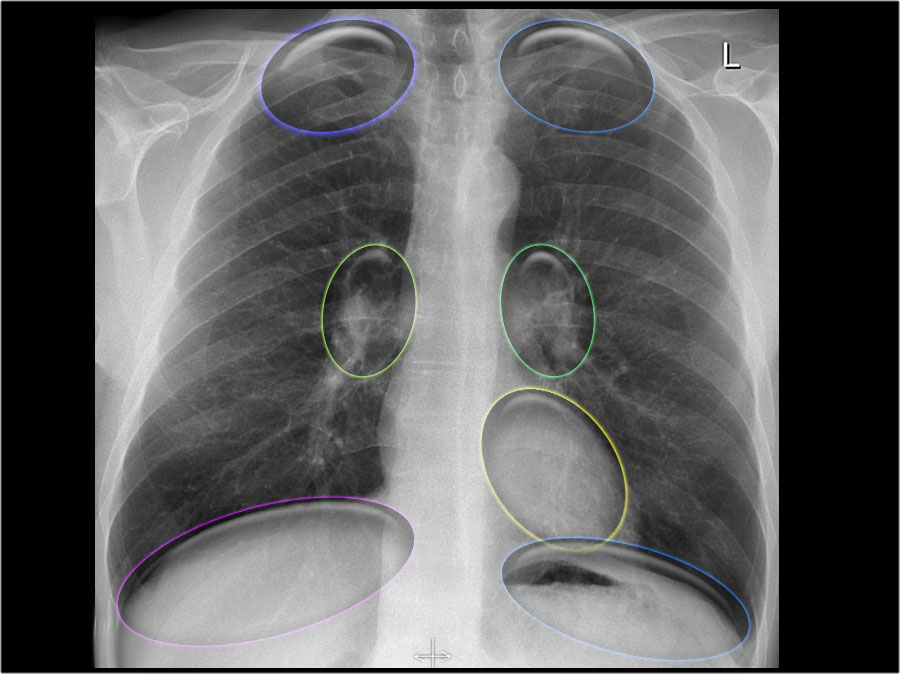
CXR
Can demonstrate signs of RV failure – enlarged RA, RV, pulmonary arteries
Can demonstrate underlying etiology – hyperinflation, ILD, edema
Echo
Best initial diagnostic test
Apical four chamber helpful to evaluate size of RV relative to LV and assess for septal deviation
US not helpful in assessing volume status in these patients!
Management
Start with ABC’s
Give home medications
If known PH consult pulmonology early
Consider 3 Ps: Preload, Pump and Pipes
RV function determined by 3Ps: Preload, Pump, Pipes
Preload:
Consider gentle hydration (250cc IVF) vs. gentle diuresis
Pump:
Cardiovert dysrhythmias as indicated
Consider inotropic support
Dobutamine 2-10 mcg/kg/min
Milrinone 50mcg/kg bolus -> 0.2-0.8mcg/kg/min (can cause hypotension)
Consider low dose norepinephrine (0.05–0.75mcg/kg/min) to maintain coronary artery perfusion
Pipes: (afterload)
Consider Pulmonary vasodilators
Prostanoids, endothelin receptor antagonists, and phosphodiesterase-5 (PDE-5) inhibitors
Prostanoids are treatment of choice
Epoprostenol is the only therapy proven to improve survival
inhaled nitric oxide 20-40ppm (good in bypass, doesn’t cause systemic hypotension as inactivated when bound to Hb)
Treat underlying etiologies
If need to provide respiratory support consider doing it in consultation with pt’s pulmonologist:
Always start with NRB before positive pressure ventilation (PPV)
PPV can cause rapid cardiovascular collapse due to increased Pulmonary Vascular Resistance and decreased preload
If you must intubate, have vasopressors at bedside: phenylepherine + NE + vasopressin are all OK
Low TV, low PEEP ventilation strategy
aggressively treat hypercarbia, acidosis, hypothermia (all increase PVR), which can increase pulmonary vascular resistance, pulmonary artery pressure, and RV strain
References: LITFL, EMDocs, UpToDate
,