Hi there, it's your friendly neighborhood admin/teaching resident and today for Trauma Tuesday we'll be talking in general about whole-body CT (or "pan-scan") for polytrauma patients, and in specific about an institutional protocol for whole-body CT that is used at the Shock Trauma Center at UMD Baltimore. For those who have ever had the pleasure of rotating at STC, this might be more-familiarly called the "Shan scan".
The use of whole-body CT in polytrauma has rapidly increased in the two-odd decades since it first gained a foothold in trauma center EDs. Imagine a world where only 5% of "major trauma" patients (i.e. patients that would fall into the trauma level 1 and 2 categories here at Maimo based on mechanism, vitals, on-scene findings, etc.) get pan-scanned, but that was 2002. Whole-body CT as a term exists in contrast to selective CT imaging, wherein only regions of interest identified on exam, E-FAST, and CXR/PXR are put through cross-sectional imaging. Institutional protocols vary, but the most common battery of imaging includes non-contrast CT head, non-contrast CT C-spine, and contrast CT chest/abdomen/pelvis; additional limbs or phases can be added based on clinical needs. Depending on the protocol, whole-body CT may precede or follow the E-FAST and CXR/PXR.
Early research comparing WBCT to NWBCT mostly comprised retrospective or non-randomized studies, with numerous variations in institutional characteristics (distance to CT scanner, level of trauma center, etc.) as well as in protocols (such as timing of WBCT, whether done immediately after primary survey or after E-FAST and XRs). Meta-analyses of this phase found that WBCT had an association with decreased mortality, shorter ED stays, and shorter time to OR.
2016 would bring us the first RCT comparing WBCT to standard imaging. The European REACT-2 study compared immediate WBCT vs POCUS/XR + selective CT in adult patients presenting with potential severe injuries based on initial assessment (any of RR≥30 or ≤10, HR≥120, SBP≤100, EBL≥500ml, GCS≤13, abnormal pupil exam; or concern for ≥2 long bone fractures, multiple rib fractures, flail chest, open chest, pelvic fracture, unstable vertebral fractures, cord compression; or severe mechanism such as fall from ≥3 meters, or ejection from vehicle). In the WBCT group, CT followed any life-saving interventions (such as intubation or chest tube insertion) but preceded any POCUS or XR. In the control group, selective CT followed POCUS and XR; interestingly, nearly half of patients in the control group ended up being pan-scanned. The authors found no difference in in-hospital mortality between the groups (15.9% vs 15.7%), but did find significant timing benefits to WBCT in the form of 30 min vs 37min to completion of imaging, and 50 min vs 58 min to diagnosis; but failed to find a statistically significant improvement in time to exit of trauma bay (63 min vs 72 min). Cost of workup was similar (€24,967 vs €26,995). The WBCT group had a small but statistically significant increase in radiation dosage (20.9 mSv vs 20.6 mSv). For context, our yearly radiation exposure in the US is approximately 3 mSv/year. The risk of cancer increases above 100 mSv/year exposure, and OSHA sets a limit of 50 mSv/year for workers in radiation environments (e.g. radiology techs, uranium miners, nuclear reactor personnel).
So if you're at a level 1 trauma center like the hospitals in the REACT-2 study, and your patient is hemodynamically stable for CT, you can trust your clinical acumen and obtain CT imaging in whichever mode and timing you feel is appropriate. But don't forget about radiation — while differences in total exposure between the groups is small, an individual who receives WBCT when they might have only needed a CT head + C-spine is receiving an extra ~19 mSv, and they probably wouldn't thank you for it.
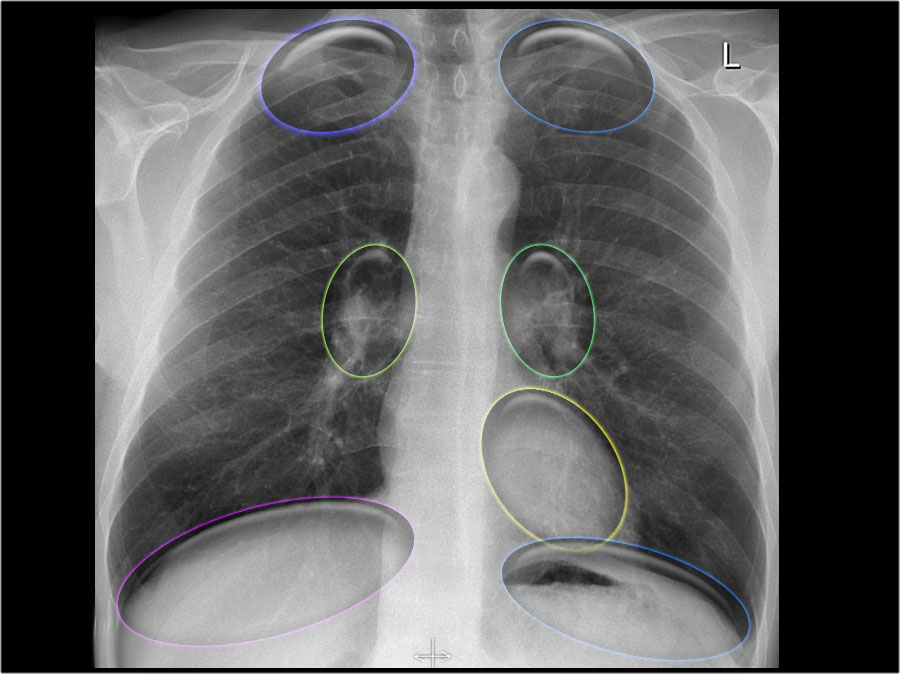
For the half of our major trauma patients who are getting a pan-scan anyway, the folks at Shock Trauma Center have their "Shan scan". This is named in honor of Dr. Kathirkamanathan Shanmuganathan (RIP), who was a Professor Diagnostic Radiology at UMD who made copious contributions to the field of trauma and emergency radiology, and was awarded the American Society of Emergency Radiology’s Gold Medal in 2014. In 2009, Dr. Shanmuganathan's group described a single-pass continuous WBCT protocol for polytrauma patients. They compared their protocol of noncontrast CT head followed by a scan from the circle of Willis through the pubic symphysis (with either monophasic or biphasic contrast injection) vs the conventional pan-scan (noncon CTH/C-spine, contrast CT C/A/P). They found that this single-pass protocol resulted in significantly decreased scan time (11.6 minutes vs 19 minutes). The time difference was attributed to decreased repositioning/management of the patient, and decreased software operation time.
Beyond shaving down vital minutes (and reducing radiation exposure by eliminating redundant/overlapping areas), the Shan scan differs from the conventional pan-scan with the addition of CT angiography of the brain and neck. This can be useful for the screening/diagnosis of cerebrovascular occlusion (stroke) as well as blunt cerebrovascular injury. Remember that trauma can be a stroke chameleon! — we've had multiple M&M presentations over the last 1.5 years about basilar artery or MCA occlusions that presented as falls with head strike and neuro deficits. Meanwhile, BCVI (carotid or vertebral artery injury) has been shown to have an incidence of 0.5-2% across all major blunt trauma patients, rising to 9% in blunt head trauma and up to 41% in severe neck injury. The risk for subsequent stroke in patients with BCVI is 20-30%, with all its associated mortality and morbidity. Anticoagulation after BCVI is identified is effective in preventing stroke; sadly, in the past, up to a third of BCVI's were only diagnosed after the manifestation of stroke symptoms.
I didn't get further into the weeds on trauma radiology studies for single-pass continuous CT with regard to overall clinical/mortality benefit, but based on anecdotal evidence I myself (as someone with a low risk tolerance) would have a low threshold to obtain a CTA head/neck as part of a trauma workup, especially if factors such as AMS or lack of collateral limit the history and exam.
References:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(09)60232-4/abstract
https://link.springer.com/article/10.1186/s13049-014-0054-2
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)30932-1/abstract
https://www.sciencedirect.com/science/article/abs/pii/S0735675717302152
https://ajronline.org/doi/pdf/10.2214/AJR.07.3702
https://link.springer.com/article/10.1186/s13049-018-0559-1
https://www.sciencedirect.com/science/article/abs/pii/S0002961099002457