Today's POTD is inspired by resident extraordinaire Dr. Doge Pologe. As usual, TL;DR is below the main text.
Thrombophlebitis is essentially a composite of two diagnoses: phlebitis, which is a clinical diagnosis in the setting of an erythema and pain overlying a vein and an identified thrombus. In the lower extremities, this is most likely to occur in varicose veins.
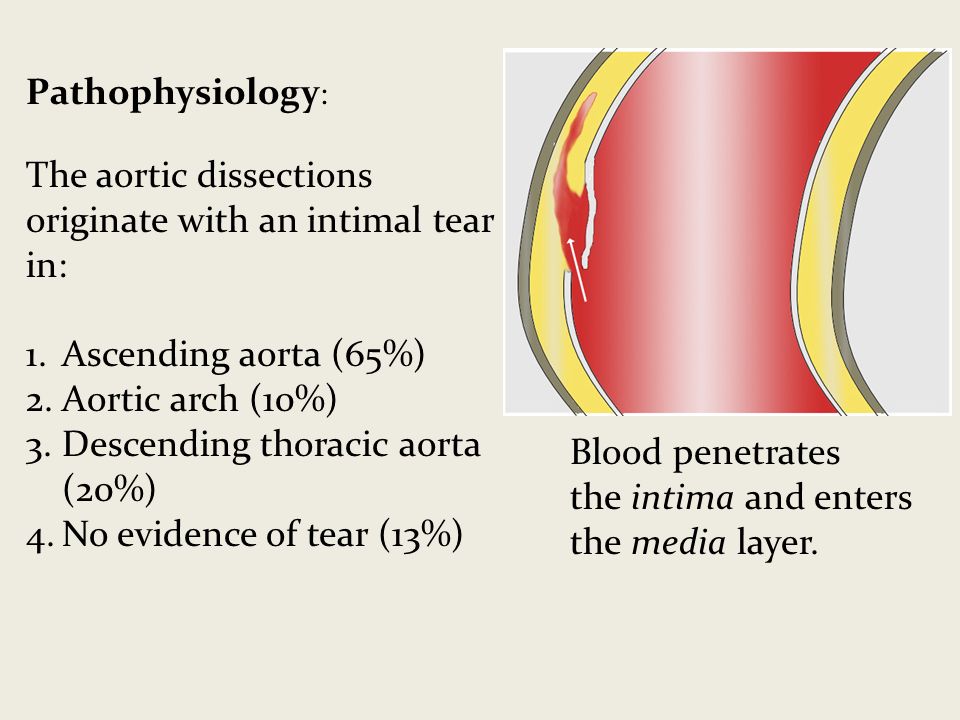
In general, risk factors for thrombophlebitis are the same as for DVT (think Virchow's Triad of hypercoagulability, hemodynamic changes (stasis/turbulence), and endothelial injury/dysfunction). These include pregnancy, history of vein excision/ablation, history of prior thrombosis, malignancy, and prior IV catheter placement.
Special cases:
"Mondor": thrombophlebitis of a breast vein, anterior chest vein, or of the dorsal penile vein. The two former should prompt a search for breast cancer and the later is usually due to repetitive trauma
"Trousseau's sign of malignancy": migratory thromboembolism, has a strong association with adenocarcinoma of the pancreas and lung
Diagnosis:
Diagnosis of phlebitis is clinical. Ultrasound should be used to identify a thrombus to distinguish between phlebitis and thrombophlebitis. Patients should also have duplex ultrasound to identify a DVT especially if the area of concern is above the knee. This is important because the rate of concurrent DVT in all cases is 25% and the rate of concurrent PE is 5%.
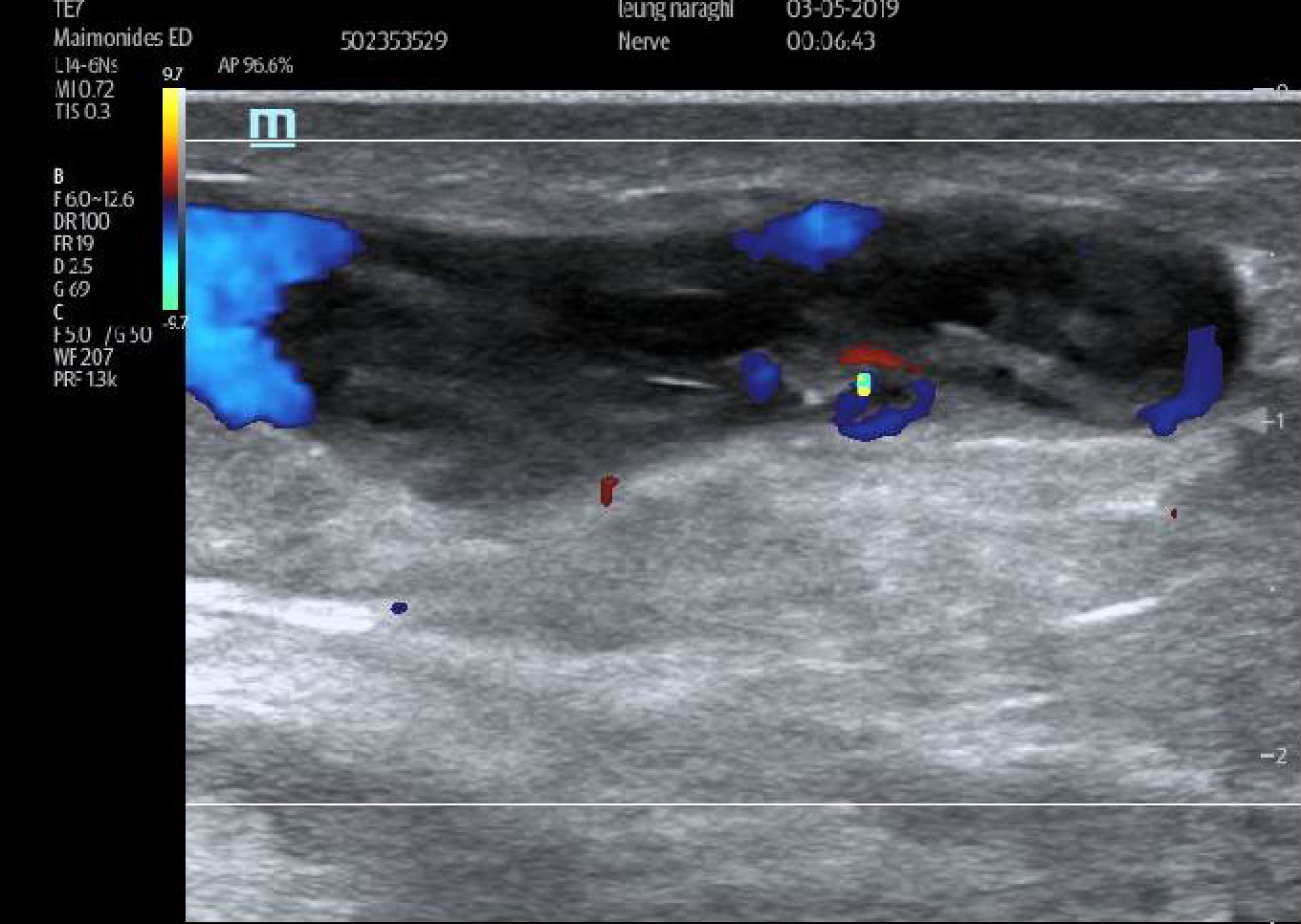
Thrombophlebitis on ultrasound will demonstrate heterogeneous internal echoes within a superficial vein. Unlike an abscess or a lymph node, this will not be discrete and you should be able to trace it out. in the words of the Doge:
"it looks like a weird continuous twisty spaghetti
abscess thing;
but it's not to be feared,
mostly superfluous, so get frisky and ultrasound that biddy,
color doppler, diagnosis, ka-ching".
There may be flow present (which can help distinguish an abscess from thrombophlebitis; abscess = no flow). Some examples (by the Doge Pologe and myself):
Treatment:
As with treatment of below the knee VTE, the treatment of superficial thrombophlebitis is controversial. Patients can be considered low risk (for VTE) if they meet these criteria:
Affected vein segment < 5cm
Remote from the saphenofemoral/saphenopopliteal junction
Low risk for VTE
**Repeat duplex should be obtained in 7-10 days or for worsening symptoms to check for propagation!
NB: thrombophlebitis post-ablation are always low risk and do not require treatment
For these uncomplicated cases, treatment is aimed at alleviating symptoms and prevention of propagation. This includes the following:
NSAIDs
Warm/cool compresses
Elevation of the extremity
Compression stockings
Patients that do not qualify as low risk or if they have recurrent thromboembolism should be considered for anticoagulation. Although studies looking at anticoagulation for SVT are small and flawed, NSAIDs, LMWH, and fondaparinux have all been shown to decrease incidence of DVT. Patients can also be discharged on Xarelto (this is the only NOAC to be studied for this indication).
In addition, thromboembolism can become suppurative. Signs and symptoms include high fever (as opposed to the low-grade fever that accompany simple thrombophlebitis) and purulent drainage (duh). In these cases, consider antibiotics.
TL;DR
Thrombophlebitis = phlebitis (redness/pain along vein) + thrombus
Find the thrombus on ultrasound! Look for internal echoes.
Low risk patients = below the knee, affected vein < 5cm, distance remove from saphenofemoral/saphenopopliteal junction can be managed with NSAIDs, compression stockings, warm/cool compresses, elevation
Low risk patients should get repeat study in 7-10 days to check for propagation
High risk patients: consider anticoagulation with LWMH, fondaparinux, or Xarelto
Antibiotics for suppurative thrombophlebitis
Special thanks to Dr. Jonas Pologe, Dr. Lawrence Haines, and Dr. Leily Naraghi Bagher Pour.
Sources:
http://www.emdocs.net/core-em-superficial-venous-thrombosis-svt/
https://www.bmj.com/rapid-response/2011/10/31/superficial-thrombophlebitis-not-straightforward-we-may-think
https://emedicine.medscape.com/article/463256-overview
https://www.uptodate.com/contents/phlebitis-and-thrombosis-of-the-superficial-lower-extremity-veins
https://radiopaedia.org/cases/superficial-thrombophlebitis-1?lang=us