Resuscitation of the Pregnant Trauma patient
General principles
· Trauma is the most common cause of non-obstetrical maternal death in the United States
· Best fetal resuscitation is good maternal resuscitation.
· Stabilization of the pregnant women is the first priority; then, if the fetus is viable (≥ 23 weeks), fetal heart rate auscultation and fetal monitoring can be initiated and an obstetrical consultation obtained as soon as feasible
· In Rh-negative pregnant trauma patients, quantification of maternal–fetal hemorrhage by tests such as Kleihauer-Betke should be done to determine the need for additional doses of anti-D immunoglobulin.
· Tetanus vaccination is safe in pregnancy and should be given when indicated.
Airway
· Greater risk for difficult intubation than non-pregnant patient
· Pregnancy related changes à decreased functional residual capacity, reduced respiratory system compliance, increased airway resistance, and increased oxygen requirements
· Gastric emptying is delayed in pregnancy à greater risk for aspiration
· Respiratory tract mucosal edema à A smaller size of endotracheal tube is recommended
· Choice of RSI medications NOT affected by pregnancy status
Breathing
· Place chest tube one to 2 intercostal spaces higher than usual to account for displacement of the diaphragm during pregnancy
· Marked increases in basal oxygen consumption à lower threshold for supplemental oxygen
Circulation
· Fluid and Colloid resuscitation like standard trauma protocol
· Uteroplacental vasculature is highly responsive to vasopressors, and their administration may decrease placental perfusion à vasopressors should be avoided unless refractory
· Avoid supine hypotension: Compression of IVC by the uterus can cause up to 30% reduction in cardiac output à Place in left lateral position or by manual displacement of the uterus while the injured patient is secured in the supine position
· O-negative blood should be transfused in order to avoid Rh sensitization in Rh-negative women
· Vital signs: heart rate increases by 15% during pregnancy. Tachycardia and hypotension, typical of hypovolemic shock, may appear late in the pregnant trauma patient because of her increased blood volume.
· Maternal vital signs and perfusion may be preserved at the expense of uteroplacental perfusion, delaying the occurrence of signs of hypovolemic shock
· Attempt to obtain supra-diaphragmatic intravenous or intraosseous access for volume resuscitation and medication administration.
FAST
· The FAST is less sensitive for free fluid in the pregnant patient than in non-pregnant patients. Sensitivity decreases with increasing gestational age, likely due to altered fluid flow within the abdomen.
· Management of suspected placental abruption should not be delayed pending confirmation by ultrasonography as ultrasound is not a sensitive tool for its diagnosis.
Secondary survey
· In cases of vaginal bleeding at or after 23 weeks, speculum or digital vaginal examination should be deferred until placenta previa is excluded by a prior or current ultrasound scan.
Imaging
· Radiographic studies indicated for maternal evaluation including abdominal computed tomography should not be deferred or delayed due to concerns regarding fetal exposure to radiation.
· Ionizing radiation has the highest teratogenic potential during the period of organogenesis (5–10 weeks), with an increased risk of miscarriage before this period.
· With abdominal CT during the third trimester the fetal exposure is around 3.5 rads, which is still under the threshold for fetal damage
· Contrast agents should be used if indicated.
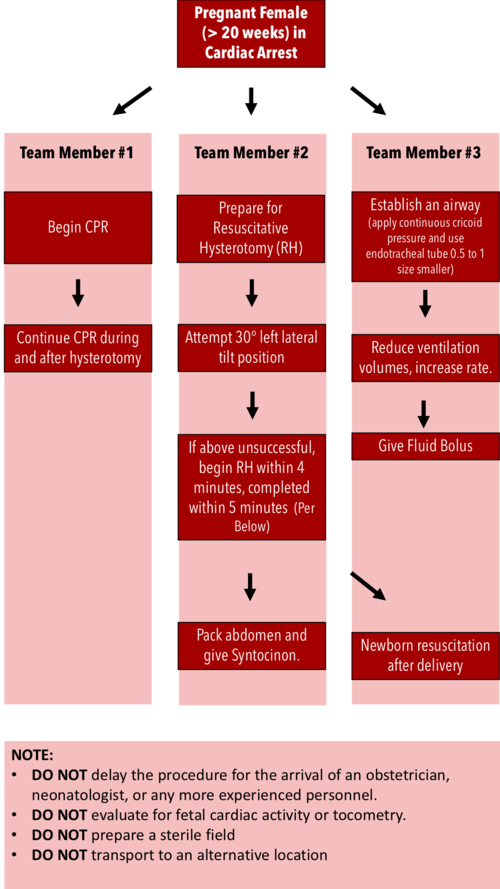
Resuscitative Hysterotomy in Cardiac Arrest
· Should begin within 4 minutes and completed within 5 minutes of cardiac arrest
· Both maternal and fetal survival decrease significantly after 5 minutes
· Do NOT delay the procedure for the arrival of an obstetrician or neonatologist.
· Do NOT evaluate for fetal cardiac activity or tocometry.
· Do NOT prepare a sterile field (but be as clean as possible).
· Do NOT transport to an alternative location.
· Performing RH increases maternal cardiac output by 30%.