For those of you following along from PSA Part 1...the answer to the question at the end is ketamine!
For Part 2, we’ll be discussing the most commonly used Procedural Sedation and Analgesia (PSA) agents including their classifications, recommended doses, peak effects, durations, and some comments that I think are noteworthy about each of them as they relate to PSA. And yes there's more than just ketamine!
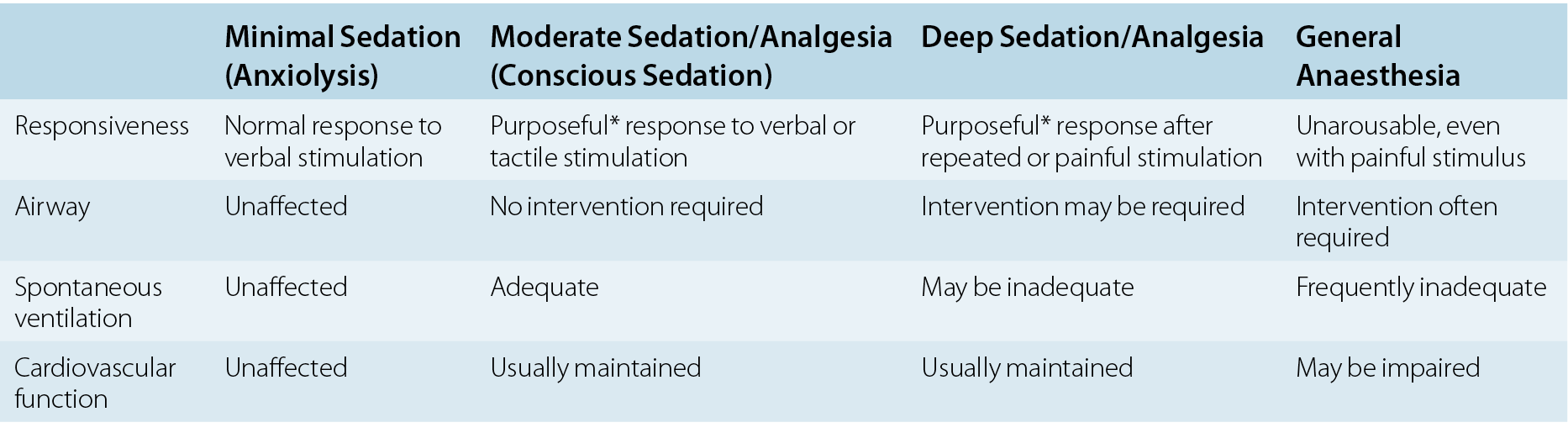
Remember for our purposes when we discuss PSA, our goal is usually moderate to deep sedation!
Commonly used agents:
Midazolam (Benzodiazepine)
anxiolytic, sedative, amnestic, muscle relaxant, anticonvulsant
Dose: 0.05 - 0.1 mg/kg IV; 0.1mg/kg IM
Peak effect: 2-3 mins IV; 15-30 mins IM
Duration: 20-30 mins IV; 1-2h IM
Comments: May produce paradoxical excitement.
Can use flumazenil as a reversal agent.
Does not provide analgesia (sometimes given with opioid).
Can cause hypotension and respiratory depression.
Fentanyl (Opioid)
analgesic
Dose: 1 - 3 mcg/kg IV
Peak effect: 2-3 mins
Duration: 30-60 mins
Comments: Typically used in conjunction with another agent for pain relief.
100 times more potent than morphine but much shorter acting.
Relatively safe hemodynamic profile, rarely causes hypotension.
Can cause respiratory depression.
Can use naloxone as a reversal agent.
Commonly observed reaction is nasal pruritus so patients will try to scratch their nose.
Rare but serious side effect to remember is that it can cause Rigid Chest Syndrome, usually in pediatrics and usually with larger doses. Can attempt rescue ventilation in this case but will likely need to reverse with naloxone or possibly give paralytic and intubate.
Can give intranasally for immediate pain relief prior to a PSA and if applicable, before IV access is established (more commonly done in pediatrics).
Pentobarbital (barbiturate)
sedative, amnestic, anticonvulsant
Dose: 2.5 mg/kg IV
Peak effect: 3-5 mins
Duration: 15 mins
Comments: Can lead to respiratory depression and hypotension.
Apparently the IV sedative of choice for children in many diagnostic imaging centers for its quick onset and short duration of action and considered superior to midazolam.
Ketamine (NMDA receptor antagonist)
dissociative, analgesic, amnestic
Dose: 1mg/kg IV; 4mg/kg IM
Peak effect: 1-3 mins IV; 5-20 mins IM
Duration: 15-30 mins IV; 30-60 mins IM
Comments: Everyone’s favorite in EM and probably deserves its very own post.
Not considered a sedative in the classic sense because of its dissociative properties.
Can cause bronchodilation and bronchorrhea resulting in excessive salivation.
Can cause transient apnea and transient laryngospasm. If suspecting laryngospasm, can try jaw thrust using the laryngospasm notch maneuver. If that doesn’t work can try bagging through. If still unable to ventilate, will need to give paralytic and intubate.
Can cause a profound emergence reaction and is contraindicated in patients with schizophrenia and psychosis. Emergence reaction is less common in pediatric patients. One way to prevent this recovery agitation is by helping the patient go into the “K-Hole” smoothly prior to and during medication administration by helping them think happy thoughts, having them think of their favorite place, or maybe even doing some magic therapy (for more info: www.magic-aid.org). If patient is having a very agitated emergence reaction and calmly talking to them/trying to redirect them does not work, can give a dose of midazolam or propofol to help calm them. Would not recommend magic therapy on a patient with emergence reaction.
Can cause emesis, typically in the recovery phase. Can give ondansetron in recovery phase. No evidence that co-administration of ondansetron with ketamine reduces incidence of nausea in recovery phase.
Can cause muscle rigidity.
Typically pushed slowly but no evidence to show that this reduces incidence of laryngospasm or nausea, contrary to popular belief.
Sympathomimetic properties which cause inhibition of catecholamine reuptake results in increase in blood pressure and heart rate. This means that in a critically ill patient who is on multiple pressors and is out of native catecholamines, ketamine actually causes myocardial depression.
Can give IM before IV access is established and maybe not even start an IV if you don't need one (more commonly done in pediatrics).
Etomidate (GABA agonist, positive modulator of GABA receptor)
sedative, anxiolytic
Dose: 0.15 mg/kg IV
Peak effect: 15-30 secs
Duration: 3-8 mins
Comments: No analgesic property.
Hemodynamically stable.
Fast-on and fast-off.
Can possibly cause adrenal suppression in septic patients although likely irrelevant for one time dose for PSA.
Can cause respiratory depression, myoclonus, vomiting.
Can lower seizure threshold. Do not give to someone with epilepsy.
Propofol (positive modulator of GABA receptor)
sedative, anxiolytic
Dose: 0.5 - 1 mg/kg IV
Peak effect: 30-60 secs
Duration: 5-6 mins
Comments: No analgesic property.
Hurts going into vein, can pretreat with lidocaine or mix with lidocaine.
Can cause transient apnea, respiratory depression, hypotension.
Fast-on and fast-off.
Can cause muscle relaxation
Common teaching has been to avoid in patients with known or suspected allergy to eggs or soy products but this has been debunked.
“Ketofol” (combination of ketamine and propofol)
Dose: ketamine 0.125-0.5mg/kg + propofol 0.5mg/kg IV
Peak effect: 30-60 secs
Duration: 15 mins
Comments: Can either give 1:1 or give subdissociative dose of ketamine with PSA dose propofol.
These agents supplement each other: ketamine mitigates propofol-induced hypotension and propofol mitigates ketamine-induced vomiting and recovery agitation.
Some commonly encountered procedures requiring PSA and what I like to use (just in general, always take into account specific patient factors):
Cardioversion = etomidate + fentanyl
Complicated pediatric laceration repair: ketamine
Fracture/Joint reduction (recently dislocated): ketamine
Adult Joint reduction (delayed presentation): ketamine + propofol
What are your thoughts? Do you have any favorite go-to procedure-drug pairings?
Stay tuned for PSA Part 3 where we put everything together and discuss the setup and procedure!