Studies show that about 10% of US women aged 15-49 use long acting reversible contraception (LARCs) and many of those happen to be intrauterine devices, or IUDs.
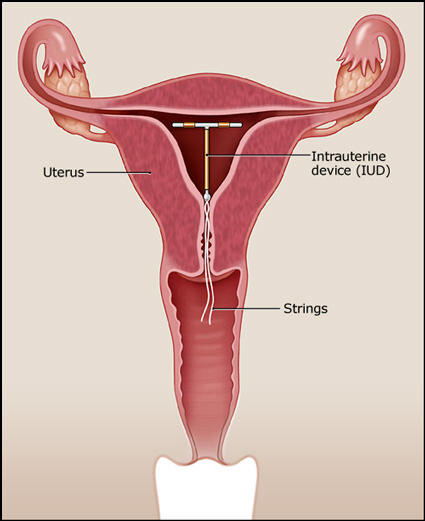
IUDs are a small flexible T-shaped piece of plastic that sit in the uterus and are used for contraception.
What do we as Emergency providers have to know about IUDs and when is it an emergency?
There are 2 categories of IUDs: copper and hormonal.
5 brands are approved for use in the US.
ParaGard (copper)
works by causing an inflammatory response which impairs movement and viability of sperm and diminishes the ability of a fertilized egg to implant
can be used for 10 years
women experience heavy periods/more cramping
string color is clear or white
Mirena, Liletta, Skyla, Kyleena (hormone)
works by releasing a progestin hormone which thickens the cervical mucus, thins uterine wall, and impairs binding of sperm to the egg
can be used for 3-5 years depending on the brand
women experience lighter periods/less cramps
string color is blue or brown
Complications are most commonly see within 1 month of placement and include PID, expulsion, perforation of uterus.
How to evaluate a patient with an IUD coming in with lower abdominal/pelvic complaints:
On exam, look for the IUD strings. There are 2 but they can appear as 1. They are generally 2.5cm in length.
If the strings are too short or not visible at all:
The strings might be curled up in the cervix. Take a cytobrush or Q-tip and sweep the os to see if you can uncurl the strings.
If you still can't see the strings, perform a bedside ultrasound.
If the IUD is in the right location but there are no strings visible, provide outpatient OBGYN follow up.
If the IUD is visible on ultrasound but not in the right location, it might have perforated the uterus. Call OBGYN to evaluate the patient.
If the IUD is not visible on ultrasound, it might have perforated entirely through the uterus. Perform a KUB to make sure it is not somewhere else in the abdomen. If you see it on KUB, again call OBGYN.
If you don't see it on KUB, it's possible that the IUD has fallen out of the uterus. Provide outpatient OBGYN follow up.
If the strings are too long or absent and the IUD is partially out, remove the IUD completely.
If the patient has PID, treat it the same way you would if the patient did not have an IUD and provide OBGYN follow up. Although not removing an IUD in this case goes against logical sense, studies have shown that women who retained their IUDs had similar or better outcomes than women who had their IUDs removed.
Definitely still perform a pregnancy test. There is a 0.1-1.5% risk of pregnancy, depending on which brand of IUD. If the patient is pregnant, be very worried about an ectopic pregnancy and evaluate for it!
If the patient wants to keep her pregnancy and you see an IUP on ultrasound, keep the IUD in and provide OBGYN follow up, assuming patient is otherwise stable and ready to be discharged. Removing the IUD may actually disrupt the pregnancy.
If there is no IUP and patient is stable, asymptomatic, and being discharged, be sure to provide urgent OBGYN follow up.
To remove the IUD, you can use a pair of forceps to pull on the strings. There should be no resistance. If you meet any resistance, stop and call OBGYN.
When removing an IUD, remember to tell your patient that they can become fertile again within a couple days. If they recently had intercourse, sperm can be viable for 5 days, so offer them a Plan B pill.