When to tap?
When you have a debilitating ankle injury with swelling at the tibiotalar joint preventing range of motion at that joint ie: dorsiflexion/plantarflexion.
What about the differential?
Ankle arthrocentesis allows for rapid identification of septic arthritis vs. gout vs. pseudogout vs. osteoarthritis vs. rheumatoid arthritis.
What are your landmarks?
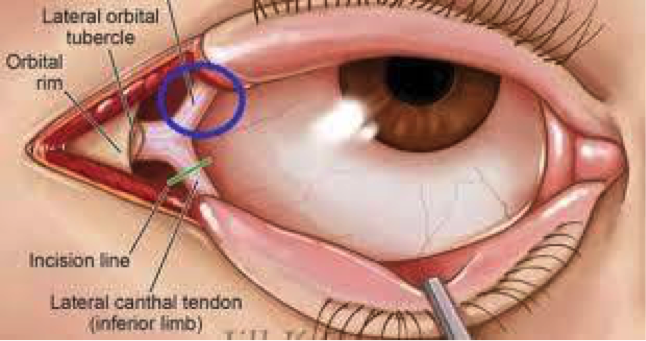
The goal is to avoid the Dorsalis pedal artery, the peroneal nerve and the tendon of the Extensor Hallucis Longus (EHL). It is recommended to use an anterolateral approach where the joint line can be found between the lateral edge of the EDL and the medial edge of the lateral malleolus (Yellow Arrow Image 1). Plantarflex the ankle while the patient is bent at the knee in the supine position to widen the joint space prior to performing the procedure.
IMAGE 1:
How do you perform it?
1. Patient should be in a supine position with the ankle in plantar flexion with plantar surface flat on the bed.
2. Mark you landmarks (see above).
3. Prepare the site (ex. chloraprep)
4. Anesthetize the area with smaller needle(23/25 gauge) creating a wheal and then advance creating the start of a projected path towards the joint capsule.
5. Attach a 5 or 10 cc syringe to a 20 or 22 gauge needle and advance the needle into the joint space pulling negative pressure as you advance. The needle should be directed perpendicular to the tibia. If your syringe starts to fill up, and you need to get more fluid out, change out your syringe using hemostats to hold the needle. Most wrist and ankle effusions will yield only 1-3cc of fluid.
What about Ultrasound Guidance?
YES. This can absolutely be used to assist you in performing the procedure and will allow for visualization of your needle tip during aspiration.
For ultrasound guidance an anteromedial approach is generally used.
Landmarks- Place probe in between the TA tendon and EHL tendon, then rotate longitudinally with the probe marker facing the patient’s head (Blue Arrow IMAGE 1). You will actually be inserting your needle medial to the TA tendon (Red Arrow IMAGE 1).
Image 2:
Image 3:
What are the relative contraindications?
Cellulitis, Adjacent osteomyelitis, Coagulopathy, Prosthetic joint, Acute fracture
Sources:
https://www.nuemblog.com/blog/ankle-arthrocentesis
(Image 1, Image 3) http://www.tamingthesru.com/blog/mastering-minor-care/ankle-arthrocentesis