Hi everyone! For today's POTD, let's think outside the box when it comes to acute headache management in the ED. Headaches in general are one of the most common chief complaints we see in the ED. We have our tried-and-true drug cocktails -- an antidopaminergic drug (ex: reglan, phenergan, compazine), +/- benadryl, +/- toradol -- but what happens if those fail?

1) Other drug therapies: a) Sumatriptan 6 mg subcutaneously, or 10-20 mg intranasally [exercise caution in pts with cardiovascular disease] b) Dihydroergotamine 0.5-1 mg IM or IV [nausea is common; also exercise caution in pts with cardiovascular risk factors] c) Valproic acid: 300-1200 mg IV
2) Sphenopalatine ganglion block: Decent amount of anecdotal support for its efficacy (although no large studies yet), and very easy to do! - Soak long cotton-tipped applicators in your choice of local anesthetic - Insert nasally and apply firm pressure until you meet resistance at the posterior wall of the nasopharynx - Leave in place for 5-10 min; bask in the glory of your migraine-stopping powers https://www.aliem.com/2017/03/trick-sphenopalatine-ganglion-block-primary-headaches/

3) Occipital nerve block: https://www.youtube.com/watch?v=JGLOaZpZwqU - Consider this for patients with primarily occipital distribution of their pain! - 1 mL of 0.5% bupivacaine injected over the greater and/or lesser occipital nerves (located along the imaginary line between the occipital protuberance and the mastoid process, as shown in this photo)

4) Cervical paraspinous nerve block: https://www.youtube.com/watch?v=oy1lggvxV9Y - Similar concept to the occipital nerve block; consider this for your cervicogenic headache patients - 1.5 mL of 0.5% bupivacaine injected approx 2-3 cm bilaterally to C6-C7, to a depth of 1-1.5 inches

References: https://www.aliem.com/2016/05/managing-migraine-headaches-complicated-patients/ http://www.emdocs.net/headache-management-best-current-evidence-ed/ http://rebelem.com/alternative-headache-therapies/ http://www.annemergmed.com/article/S0196-0644(16)30301-8/pdf https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3737484/

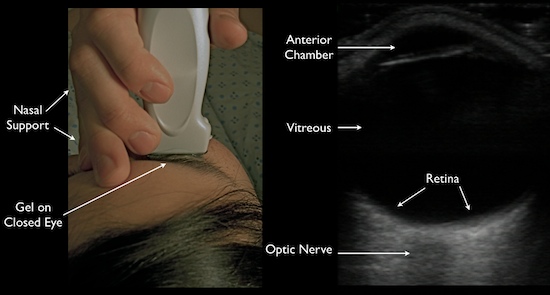


 A vitreous detachment is typically seen floating above and NOT connected to the optic nerve. It is often also hazier and swirlier (very technical terms), especially as the patient looks in different directions.
A vitreous detachment is typically seen floating above and NOT connected to the optic nerve. It is often also hazier and swirlier (very technical terms), especially as the patient looks in different directions.