Mechanism:
High-energy:
- Usually from MVC (dashboard injury resulting in axial load to flexed knee) or fall from height
Low- energy:
- Often from athletic injury (with a rotational component)
Associated injuries:
- Vascular injury
- Nerve injury: usually common peroneal nerve injury
Types:
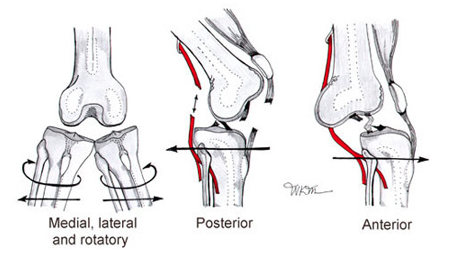
Anterior: Most common (30-50%)
- due to hyperextension injury
- usually involves tear of PCL

Posterior: 2nd most common (25%)
- due to axial load to flexed knee (dashboard injury)
- Highest rate of vascular injury (25%) – with complete tear of the popliteal artery

Lateral (13%)
- due to varus or valgus force
- usually involves tears of both ACL and PCL
- highest rate of peroneal nerve injury
- An anteromedial skin furrow, or “dimple sign” at the medial joint line, is suggestive of a posterolateral dislocation, which are irreducible!

Physical exam:
- no obvious deformity- 50% spontaneously reduce prior to ED arrival!
- obvious deformity:
o reduce immediately, especially if absent pulses
Management:
- considered an orthopedic emergency
- palpate the dorsalis pedis and posterior tibial pulses. Palpable pulses DON’T rule out a vascular injury
- reduce the knee
- apply longitudinal traction to the extremity (This is usually all that is required to reduce a knee)
- Anterior knee dislocations may require additional lifting of the distal femur
- Posterior dislocations may require lifting of proximal tibia to complete reduction.
- After reduction, the knee should be immobilized in a long leg posterior splint with the knee in 15- 20 degrees of flexion.
https://www.youtube.com/watch?v=aN7zDxtyHy8
- measure Ankle-Brachial Index (ABI):
- ABI > 0.9
- monitor with serial vascular exams
- ABI < 0.9
- perform a CT angio
- if arterial injury confirmed then consult vascular surgery
- Immediate surgical exploration is indicated if pulses are still absent following reduction. Ischemia time >8 hourshas amputation rates as high as 86%!
- The patient should be taken to the OR for external fixation if:
- vascular repair (takes precedence)
- open fx and open dislocation
- irreducible dislocation
- Compartment syndrome
- obese
- multi trauma patient
Sources: Ortho bullets, emdocs

