Idiopathic Intracranial Hypertension (IIH), previously known as ‘Psuedotumor Cerebri’ or ‘Benign Intracranial Hypertension’ that is actually NOT benign is a disorder characterized and defined by the clinical symptoms of increased intracranial pressure (ICP) not due to any other cause. IIH is, in some ways, a diagnosis of exclusion, as you must have negative neuroimaging and a normal CSF composition to rule out other causes of increased ICP prior to making this diagnosis. However, this is not your average “diagnosis of exclusion” since disease progression can lead to significant morbidity.
So, why must you not miss this diagnosis? Transient vision changes, which is the second most common presenting complaint (after headaches), can lead to permanent vision loss. And since this is primarily a disease of young, otherwise healthy individuals, you can understand why this is kind of a big deal.

Who gets it?
This is a disorder primarily of overweight females of childbearing age. However, it can affect individuals of all ages and males. Rapid weight gain over a short period of time is potentially a greater risk factor than obesity itself. Classically implicated medications include tetracyclines (doxycycline and minocycline), growth hormone, retinoids and OCPs.
How do these patients present?
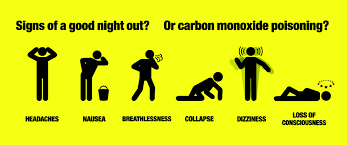
The most common complaint: Headache, often diffuse and of gradual onset, which progresses in severity over time. It is frequently accompanied by transient visual changes, which may be precipitated by positional changes (usually standing, sometimes bending forward or lying down), Valsava, eye movement or bright lights. Photopsias (a fancy term for seeing ‘brief sparkles’ or ‘flashing lights’) are frequently described. Pulsatile tinnitus, retrobulbar pain, and back pain round out the list of most frequently seen complaints.
Every complaint listed above is fairly non-specific, so this is where things get a little tricky, right? Keep this in mind: Pulsatile tinnitus (often described as hearing rushing water or wind) in the setting of new headaches is very suggestive of IIH.
Symptoms tend to wax and wane for weeks-to-months, or even years before a diagnosis is made. However, a minority of patients will have a more fulminant course with resulting rapid vision loss.
The most common abnormal findings on exam are papilledema, visual field deficits and sixth nerve palsy.

How is it diagnosed?
You MUST get neuroimaging and send CSF analysis to exclude other causes of increased ICP. And if you are considering IIH, then venous sinus thrombosis should also be on your differential—there is significant overlap in terms of presentation and risk factors.
Once you have excluded all other causes, diagnosis is made via an elevated opening pressure on that LP that you performed (lateral recumbent position).**
**Before the LP, this is the PERFECT opportunity to break out your ultrasound and measure the optic nerve diameter.
In summary, the full list of diagnostic criteria (per the Dandy criteria) are:
- Symptoms of increased ICP
- No other neurological abnormalities or impaired level of consciousness
- Elevated ICP with normal CSF composition
- Normal neuroimaging
- No other apparent cause of increased ICP
How is it treated?
For in-service: therapeutic lumbar puncture. Obviously, discontinue any potential offending agents. Weight loss, carbonic anhydrase inhibitors (acetazolamide), diuretics (furosemide) and CSF shunting are all traditionally utilized therapies. Recent data suggests that acetazolamide combined with a low-sodium, weight reduction diet may be the most effective option.
Want to learn more?
https://emedicine.medscape.com/article/1214410-overview
https://www.aao.org/eyenet/article/managing-idiopathic-intracranial-hypertension-evid
SaveSave
SaveSave
SaveSave
SaveSave