Hi everyone,
Today's POTD comes at the request of frazzled tele docs past, present, and future: how to properly request a follow-up call back in SCM.
By virtue of being a busy urban ER in NYC, we might find ourselves sending patients home with results still pending. The choice to send home a patient with pending results is a discussion between you and your God/attending, but the process of submitting a case for a call back should follow a few general principles.
4 Golden Rules of Call Backs
1) Advise patients that they will receive a call back only if there is a positive finding for results or tests. Emphasize: no news is good news! If they don't receive a call back, it means their test was negative. If the patient is persistent and still wants a call back for negative findings, then make a note of it in the Call Back Reason box.
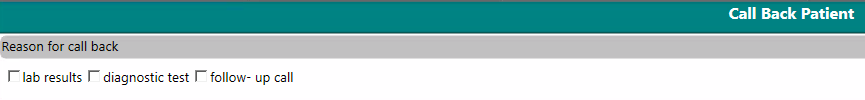
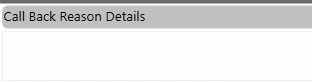
2) Specify what it is that you want the call back for in the Call Back Reason box. If you click lab results, instead of writing "lab follow-up", specify the test or value you're focused on. If you click diagnostic test, instead of writing "xray results", include which xray and what you're concerned about. If you click follow-up call, include what clinical symptoms or disease progression you're monitoring. If we don't provide a bit of context, the tele doc has to go chart digging for no reason. See below for what this looks like at the bottom of the ED Disposition Note in SCM, and compare it to what the tele doc sees on their follow-up list.
3) Do not give a call back for urine culture or STI results. The process of call backs is that the next day's tele doc gets a list of call back requests from the last 24 hours. Urine culture and STI results will inevitably not be available within 24 hours of the patient being seen, so to include next-day call back requests for these results is meaningless. However, the results of urine culture and STI testing are sent out on a regular basis to future tele docs (see below), and any positive results will automatically get a call back when they result. The only exception is that if you have high concern for STI test results, you can include it as a call back so that the tele doc can keep an eye on it.
4) Verify phone numbers! You can find a patient's phone number printed on the Discharge 123 forms below the signatures on the Patient Signature Form. It is the very first sheet in the Discharge 123 packet, and then is repeated again after the instructions and results. When you're discharging a patient, be sure to confirm the number is correct. If the number is incorrect, or especially if there is no number at all, write in the call back box the correct number.
Follow these 4 simple rules for call back requests and every tele doc will sigh in relief.
Happy calling,
Kelsey