So baby’s out, but the neonate is in trouble. It’s everyone’s worst nightmare, which is why the neonatal resuscitation protocol is there, giving clear-cut instructions for the most stressful of scenarios. Essentially, once recognizing the need for neonatal CPR, the protocol moves into standard life support algorithm instructions, with an emphasis on transport to a definitive care facility. Again, similarly to with last week’s protocol, I’ll refer to this one as a quick refresher, using it for target heart rates, respiratory rates, compression rates, and ventilation rates.
It’s a useful bit of cognitive offloading in the midst of what is otherwise emotionally overwhelming, to be sure. A protocol we hope to never have to use, but certainly one I’m grateful we have when needed.
And with that, believe it or not, we have completed the ENTIRETY of the NYC REMAC protocols!
Or at least, the current version.
SURPRISE!
In the coming weeks, a BRAND NEW version will be hitting your inboxes as well as the streets! This new iteration has been in the works for an extraordinarily long time, and it’s bringing a LOT of overdue additions (spoilers: ketorolac!!!). Can’t wait to share it all with you, but if you’d like a jumpstart on all the new goodness, you can always head to www.nycremsco.org !
Dave
- Medications
- Pharmacology
- Respiratory / Pulm
- POCUS
- Infectious Disease
- Ophthalmology
- Airway
- Obstetrics / Gynecology
- Environmental
- Procedures
- Foreign Body
- Pediatrics
- Cardiovascular
- EKG
- Critical Care
- Radiology
- Emergency
- Admin
- Orthopedics
- Nerve Blocks
- DVT
- Finance
- EMS
- Benzodiazepines
- Neurology
- Medical Legal
- Psychiatry
- Anal Fissure
- Hemorroids
- Bupivacaine
- Ropivacaine
- EM
- Neck Trauma
- Emergency Medicine
- Maisonneuve Fracture
- Diverticulitis
- Corneal Foreign Body
- Gabapentin
- Lethal Analgesic Dyad
- Opioids
- Galea Laceration
- Dialysis Catheter
- Second Victim Syndrome
- Nasal Septal Hematoma
- Nephrology / Renal
- Hematology / Oncology
- Dental / ENT
- Dermatology
- Endocrine
- Gastroenterology
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- May 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
POTD: "Push-pull" boluses - keep them sterile!
How do I appropriately use the push-pull technique to deliver a bolus to a pediatric patient?
Push-pull Technique
Hook up 3 way stopcock to IV tubing and attach syringe to 3rd port.
Turn off to patient, draw fluid from bag.
Turn off to bag, push bolus into patient with steady pressure.
Repeat 2-3 until full amount of bolus given.
Use
To deliver adequate fluid resuscitation in a timely fashion to pediatric patients (superior to gravity)
Similar flow rates as pressure bag, but with higher accuracy of volume
For difficult IVs, you are able to feel resistance when giving the bolus and recognize a blown vein earlier
Contamination Concern!?
A study showed that with repeated use, the contents inside the syringe may become contaminated (see fluorescein study below)
Gross!!! This implies we may unwittingly introduce bacteria into systemic circulation....
Tips for Improvement
Use syringe that is larger than the amount of the individual pushes (e.g. use a 60ml syringe to give 30ml at a time or a 20ml syringe to give 10ml at a time)
Consider wearing sterile gloves and maintain aseptic technique
Avoid touching the "ribs" (see below)
POTD Trauma Tuesday! Cordis vs Two 16 Gauge Peripheral IVs
I encountered the question from an inquisitive junior resident of whether two 16 gauge catheters would infuse blood products more quickly than a single 8.5 Fr cordis during a trauma resuscitation.
A Story Explained by Two Super Soakers
While cars and computers continue to break power records well into the 21st century, did you know the golden age of Super Soakers passed us in the late 90s?
Back then water gun companies sought to create the biggest, most obnoxious, and borderline injurious toys imaginable. As a result some of the most heinous and drenching devices were released that left you soggy and consulting plastics for a skin graft.
Using two of these legendary “toys” (read: weapons of watery destruction), I’m going to highlight a point of flow that applies to trauma.

One of the most powerful water guns was the Super Soaker CPS 2000. It was released in 1996 and launched a liter of water approximately 50 feet with a single pull of the trigger. It is vicious in its simplicity. It had a single barrel and would discharge nearly one liter per second. It would be discontinued and replaced after a year or so by weaker versions due to multiple reports of injuries. Worried mothers rejoiced in the streets. Its fastest rate: 849 mL/sec.

Later on in 2000, the Super Soaker Monster XL was unleashed. It holds a record for being the largest single-piece water blaster and was truly a marvel in 90’s technology. It came with a bipod, a 3.6L tank, and two barrels. The sad news is that though it is bigger and meaner looking, it would take 30 pumps before you would be able to use it adequately and it still did not pack the same punch as the original CPS 2000. Its shear weight alone prepared scores of millennials for the impending burden of student loans and housing debt. Its fastest rate: 591 mL/sec. Perhaps the number of barrels were to blame.
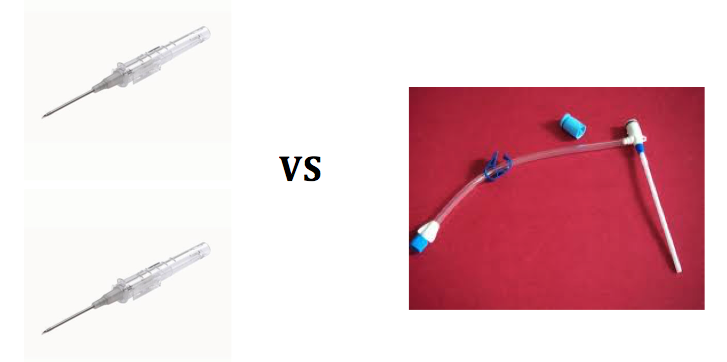
In this contest of two classic water guns, we see why the cordis has a better flow rate than other types of vascular access – say two 16 gauge needles. An ETM test (link below) using a rapid infuser found that a 7 Fr cordis can infuse one liter of fluid in under a minute. It took 46 seconds when a 8.5 Fr cordis was used. At 2.8 mm in diameter, this is approximately a 12 gauge needle in size. The 16 gauge would require two minutes and 20 seconds. Even using two lines that would be 70 seconds assuming the same conditions.
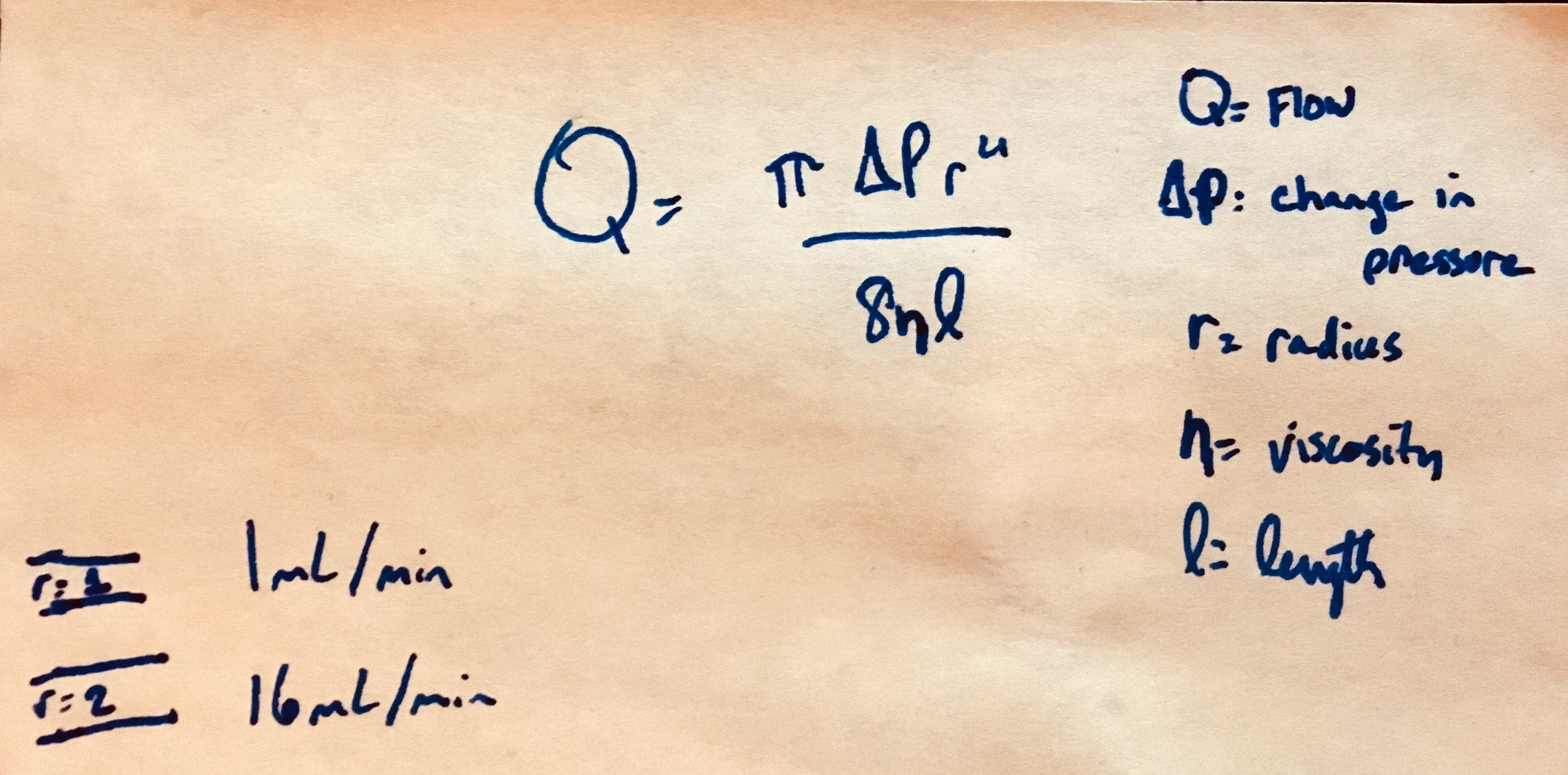
A single 16 gauge has a diameter of 1.2 mm. The difference between it and a 8.5 Fr cordis is 1.6 mm but the effect of the radius on flow is exponentially larger due to Poiseuille’s law.
Though a sufficiently intelligent rapid infuser might even the playing field, I will stick to the cordis.
Well, just to let you know how far we have come in 2018, here is a modern water gun:

Strong work generation Z. At least you still have to go outside to play with this.
Some further reading:
For the direct flow test please see ETM’s showdown: http://etmcourse.com/large-bore-iv-access-showdown/
https://icurounds65.wordpress.com/2013/11/07/venous-access-for-fluid-resuscitation-you-dont-need-a-central-line/
http://emupdates.com/2009/11/25/flow-rates-of-various-vascular-catheters/



