CODE WHITE AMBULANCE TRIAGE. The patient is at imminent risk of harming themselves and your staff. Verbal deescalation was attempted but has failed. Everyone is looking to you for your OK for chemical sedation. You dig your heels in and are about to mutter the first thing that comes to mind: "5 of haldol and 2 of ativan."
But hold up. Because this POTD is about droperidol.
Background: Droperidol is a dopamine antagonist, and is a first generation antipsychotic. It used to be a favorite of ED doctors to treat agitation in the ED and was used for more than 30 years for acute agitation. It was removed from market 20 years ago because of a black box warning due to QTC prolongation and risk of torsades/sudden cardiac death. This was based off a study looking at 273 case reports over a 4 year period. In the deaths reported, the doses used were 25mg-250mg per dose, doses MUCH higher than what we would typically give in the ED for agitation. Adverse cardiac events or death occurred in 10 patients who received a dose less than 2.5mg. From this study, the FDA placed a black box warning on droperidol. Upon further review of these cases by multiple authors, all of these cases had confounding factors that could have accounted for the adverse event. Overwhelming evidence after the FDA black box warning was issued has showed that droperidol is both safe and effective, especially when used at typical dosing for agitation.
Why Droperidol: Comparatively to other sedatives, namely haloperidol, droperidol is more potent, is faster onset, and has a shorter duration. According to Cressman et. al who examined absorption, metabolism, and excretion of droperidol, absorption via IM is near equivalent to IV administration. Onset of action is 3-10 minutes, and peaks at 30 minutes. Duration of effect is 2-4 hours, and effects may last up to 12 hours. Undergoes hepatic metabolism.
In the DORM study, 10mg droperidol IM was compared to 10mg IM Midazolam. Droperidol, compared to Midazolam, reduced the duration of violent behavior (20 min vs 24 min), required less additional sedation (33% vs 62%), and has less respiratory distress among intoxicated agitated patients.
If single agent droperidol is not enough, it was found in a study authored by Taylor et al that combination 5+5 droperidol and midazolam was more effective at sedation than droperidol or olanzapine alone.
Uses: Typical dosing ranges between 5mg -10mg for agitation, and can be administered IM or IV.
In addition, it can be used to treat headaches, vertigo, nausea, and pain, usually at half the agitation dose.
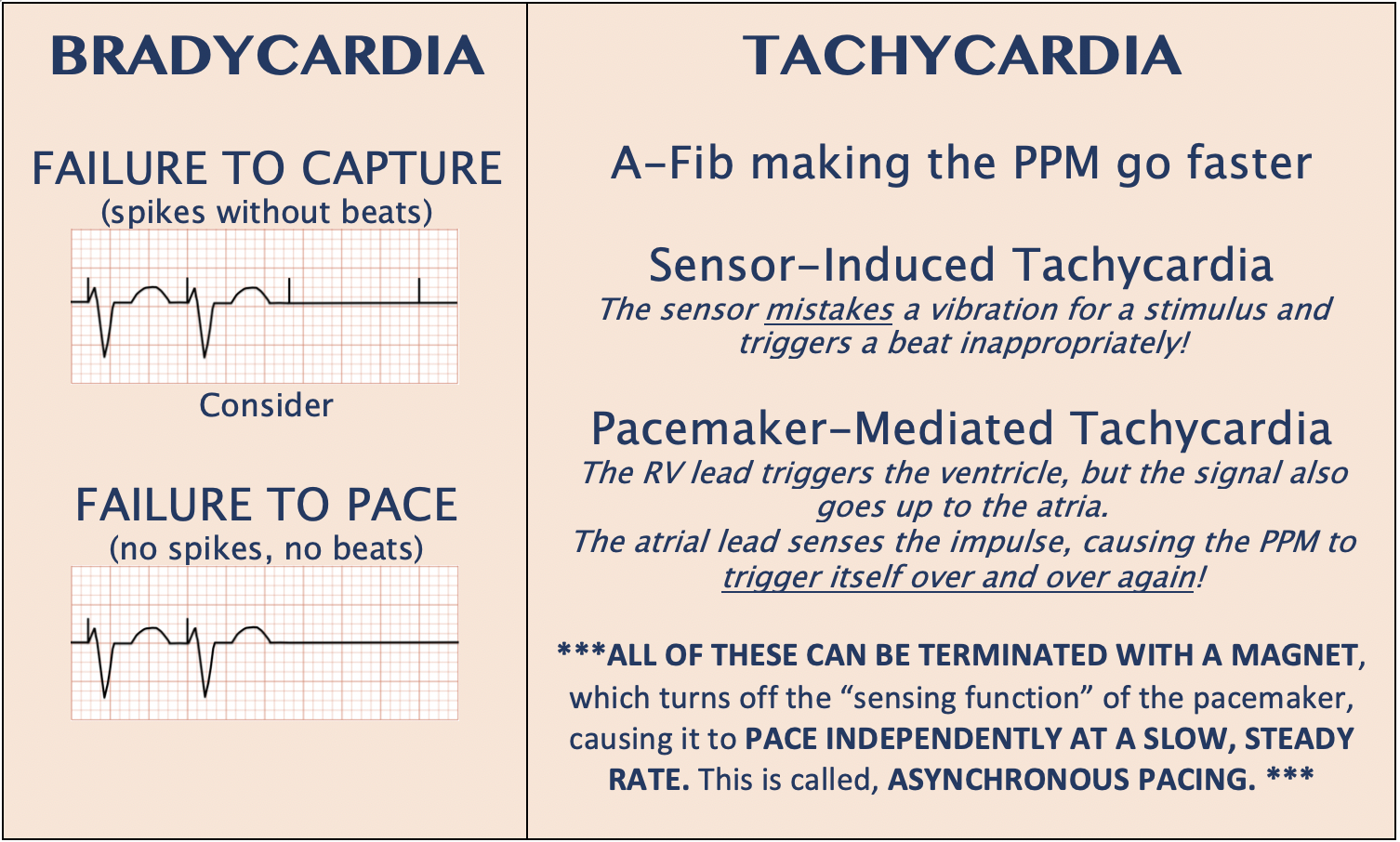
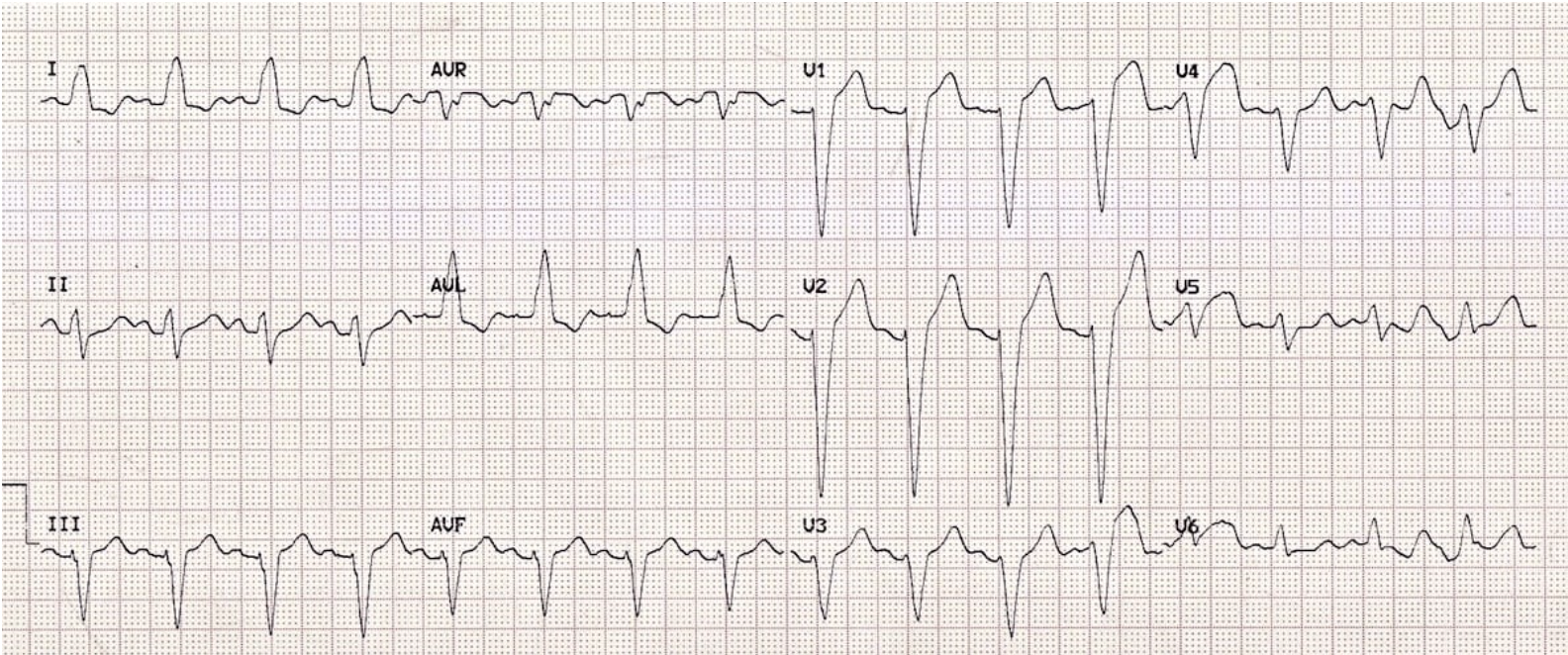
Side effects: Sedation, extrapyramidal effects, hypotension, prolongation of QT interval. Obtain an EKG if possible before administration, but if not possible, can be obtained after if the patient is agitated. Be mindful of using droperidol in the setting of patients with known prolonged QT interval and patients at risk given their medication history (e.g. methadone).
Sources:
https://pubmed.ncbi.nlm.nih.gov/4707581/
http://www.emdocs.net/droperidol-use-in-the-emergency-department-whats-old-is-new-again/
http://www.emdocs.net/the-art-of-the-ed-takedown/
https://www.tamingthesru.com/blog/2019/4/20/the-return-of-droperidol