Hello all! This week’s VOTW is brought to you by myself.
Hospital course
30 y/o M presents to the ED after 2 syncopal episodes. He had 10 days of worsening dyspnea on exertion with chest pressure and palpitations. He flew to California 1 month ago and returned yesterday.
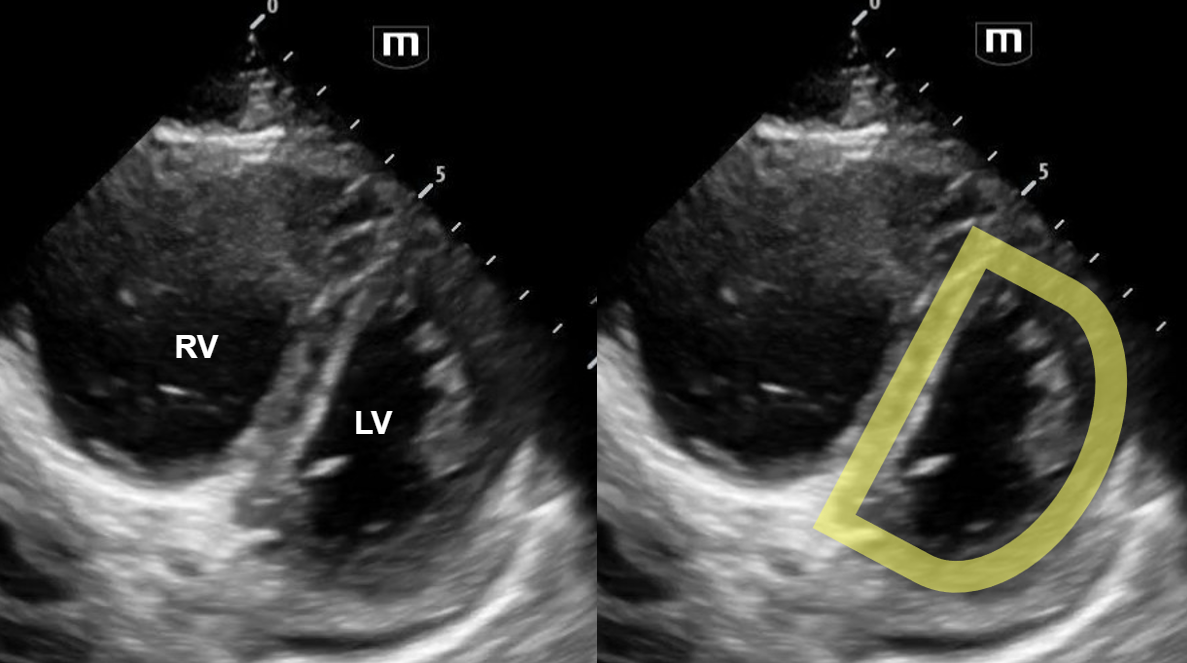
In the parasternal short view of the heart above, we see two cardiac chambers, the right ventricle (RV) and the left ventricle (LV). We can see flattening of the interventricular septum towards the LV chamber, creating a “D”-shaped LV (labelled above).
View the attached clip to see the LV take on a shape of the letter “D” with each contraction! Also note that the RV is dilated and appears larger in size than the ”D”-shaped LV.
The clip above shows a parasternal short view of a normal heart. Notice that the left ventricle appears circular, and the right ventricle forms a smaller crescent-shape surrounding the left ventricle.
Case Conclusion
CT imaging showed pulmonary emboli within the bilateral pulmonary arteries and dilatation of the right atrium and right ventricle associated with right heart strain.
Thrombectomy was deferred because patient was hemodynamically stable. He was started on a heparin infusion in the ED and then admitted.
Right heart strain
· Pulmonary embolism can cause an acute increase in pulmonary pressures and right ventricular afterload that causes increased right heart strain. Focused ultrasound has been shown to be both highly sensitive and highly specific in detecting anatomical changes of the heart seen with right heart strain.
· “D-sign” is a finding suggestive of right heart strain seen on the parasternal view of the heart. Increased right ventricular pressures cause bowing of the interventricular septum into the LV, causing the “D”-shaped LV to form.
· Other findings suggestive of right heart strain include increased RV size, McConnell’s sign, and TAPSE.
Happy scanning!
Sono team
PS: just in case nobody gets it, the subject line pun is a Simpsons reference!
Resources to review:
· https://www.thepocusatlas.com/right-ventricular-dysfunction/
· https://everydayultrasound.com/blog/category/Right+Ventricular+Strain