POTD: Eye Stuff (Trauma Tuesday!)
A.
Seidel's sign: Fluorescein stained vitreous flowing from the site of globe perforation. Should protect the globe from any external pressure with eye shield, elevate head of bed 30 degrees, analgesia, control hypertension, and prevent vomiting. Emergent Optho consult.
B.
Teardrop pupil: Usually indicated globe rupture/ FB. See management for Seidel's sign above.
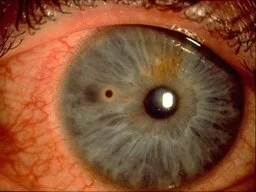
C.
Corneal foreign body with rust ring: remove foreign body, urgent follow up for rust ring removal which should be done after 24 hours from initial injury- this is because reepithelialization makes removal easier.
D.
Exophthalmos: if in setting of trauma with increased intraocular pressure suspect retrobulbar hematoma. Obtain STAT CT scan, perform STAT lateral canthotomy and emergent optho consult.
E.
Hyphema: Blood in the anterior chamber of the eye. Elevate head of bed, control intraocular pressure. Patients on anticoagulation or antiplatelet agents should be admitted for reversal and observation. Consult ophthalmology depending on size of hyphema and rebleed risk.
Stay well,
TR Adam
A.
B.
C.
D.
E.