How do I use KCentra for reversal of anticoagulation?
KCentra aka PCC4 (prothrombin complex concentrate 4)
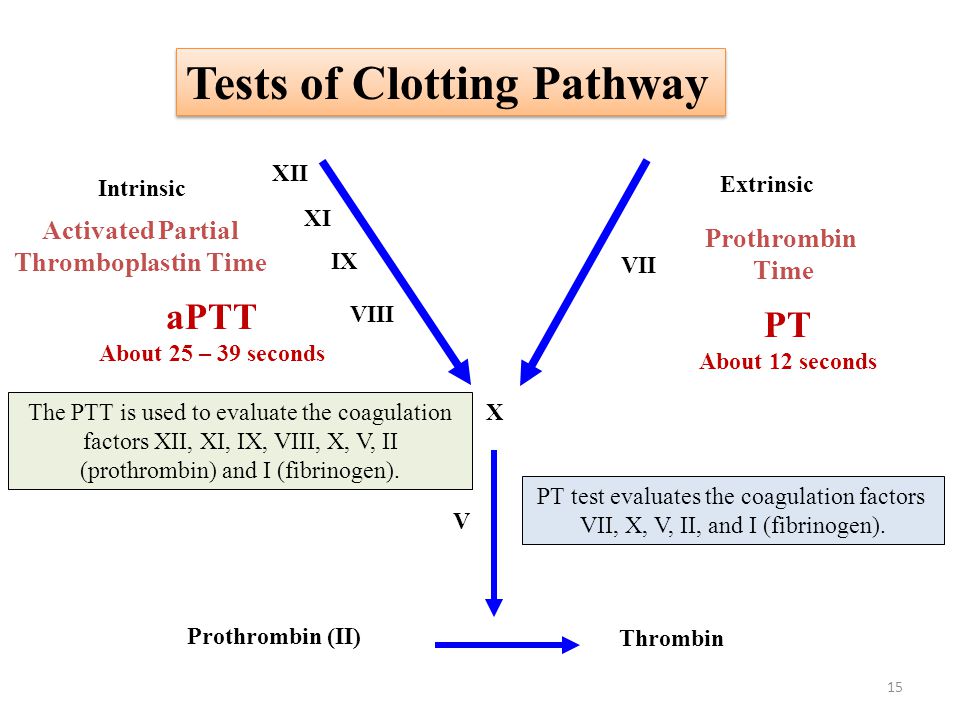
Contains Factors 2, 7, 9, 10, Proteins C & S, antithrombin III, human albumin, and heparin (to stop early activation of factors)
PCC-3 doesn't have factor 7, Protein C, or Protein S
Dosing for Warfarin Reversal
You don't have to memorize this! It's in our order set! And also on Kcentra.com
INR 2-4 = 25 units/kg
INR 4-6 = 35 units/kg
INR >6 = 50 units/kg
Life threatening bleed and don't have the INR yet? 1500 unit flat dose
MUST GET INR to assess the need for supplemental dosing.
For a 75kg patient, 1500 units is only 20 units/kg, so regardless of INR, the patient will likely require more KCentra.
Follow up
Get repeat INR 30-60 minutes after dose of KCentra
If elevated, may require additional doses
Monitor for signs and symptoms of thromboembolic events
Dosing for NOAC Reversal
50 units/kg
Contraindications
Patients with heparin induced thrombocytopenia (HIT)
Patients who do not want blood products
Also has the same risks as giving blood products