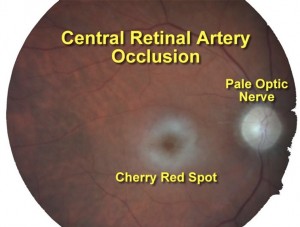
58yF with hx of CAD, DM, HTN, HLD, a-fib presents to the ED with an eye complaint - she can barely count fingers out of her left eye since this morning.

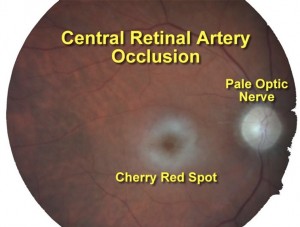
58yF with hx of CAD, DM, HTN, HLD, a-fib presents to the ED with an eye complaint - she can barely count fingers out of her left eye since this morning.

Inferior shoulder dislocation (luxatio erecta) can occur from an axial load to an outstretched arm. Imagine a swimmer hitting the side of a pool with his arm in front. Also this can occur from forced hyperabduction (grabbing something while falling). Clinically, you will notice the patient with their arm over their head and the elbow bent (fixed abduction). You may feel the humeral head in the axilla/lateral chest wall.



So a guy comes in with 16 superficial stab wounds overnight and you get to be the lucky resident to sew him up (true story). Halfway through, he starts complaining his mouth is numb (this part didn't happen). What do you do? LAST can occur from three important etiologies - direct systemic injection, accumulation from multiple injections, or injection into a highly vascularized area. Most importantly, prevent this from happening by knowing your max dose, aspirating before injecting, and asking about symptoms.
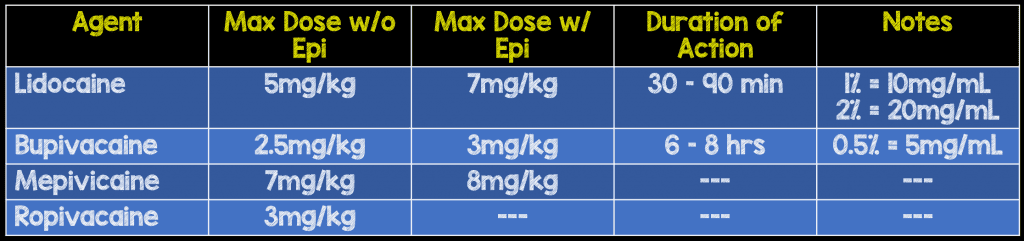 Remember local anesthetics are sodium channel blockers, so when introduced systemically cause cardiac and neuro toxicity.
Remember local anesthetics are sodium channel blockers, so when introduced systemically cause cardiac and neuro toxicity.
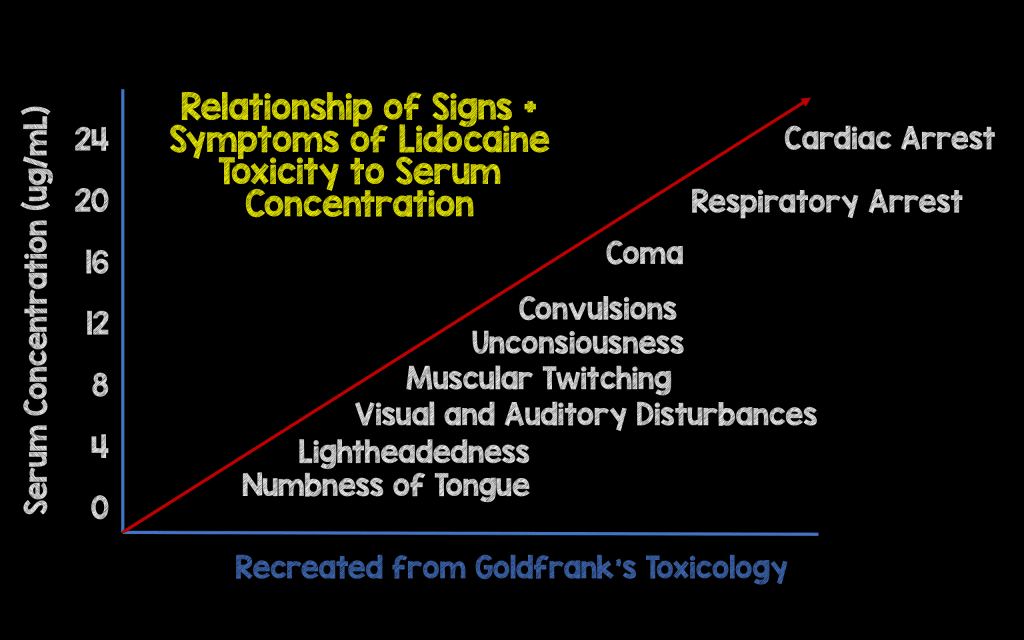
First, stop injecting the patient. Then,
A - You may need to intubate. B - Give 100% FiO2 and hyperventilate as acidosis, hypoxemia can push this syndrome into cardiac arrest. C - Hypotension should be treated with IVF and push-dose pressors (epi). In arrest, high-quality CPR should be continued for a while as these anesthetics are lipid soluble and take time to redistribute. Consider pacing and ECMO. D - Seizures can occur and benzodiazepines are the treatment, as usual.
If the patient has an arrhythmia, hemodynamic instability, prolonged seizure, or rapid progression of symptoms, break out the 20% intralipid. Call pharmacy/look up the dose - 1 ml/kg over 1 minute q3m x3 and then 0.25 ml/kg/min. Theoretically, lipid emulsion therapy works by drawing anesthetic out of the plasma.

Sources
Rebel EM: http://rebelem.com/local-anesthetic-systemic-toxicity-last/
LITFL: Local Anesthetic Toxicity
Wiki EM: Local Anesthetic Systemic Toxicity
Kapitanyan, R. Local Anesthetic Toxicity. Medscape http://emedicine.medscape.com/article/1844551-treatment#d1