Active Gastroesophageal Varices bleeding
Background:
Gastroesophageal varices bleeding is associated with a mortality rate approaching 20-30%.
Bleeding from varices stops spontaneously only in 50% of patients
Evaluation:
History:
Prior complications, medications, fever, abdominal/chest pain, vomiting, melena, syncope/pre-syncope, hematemesis, cause of cirrhosis, prior interventions on varices, weights.
Exam:
Evaluate hemodynamic status immediately (consider use of beta blockers).
Look for signs of chronic liver disease – spider angiomata, palmar erythema, jaundice, ascites (shifting dullness, fluid wave, etc.), coagulopathy (petechiae, purpura), ENT exam (pharynx), CV, pulmonary, extremities, mental status.
Labs:
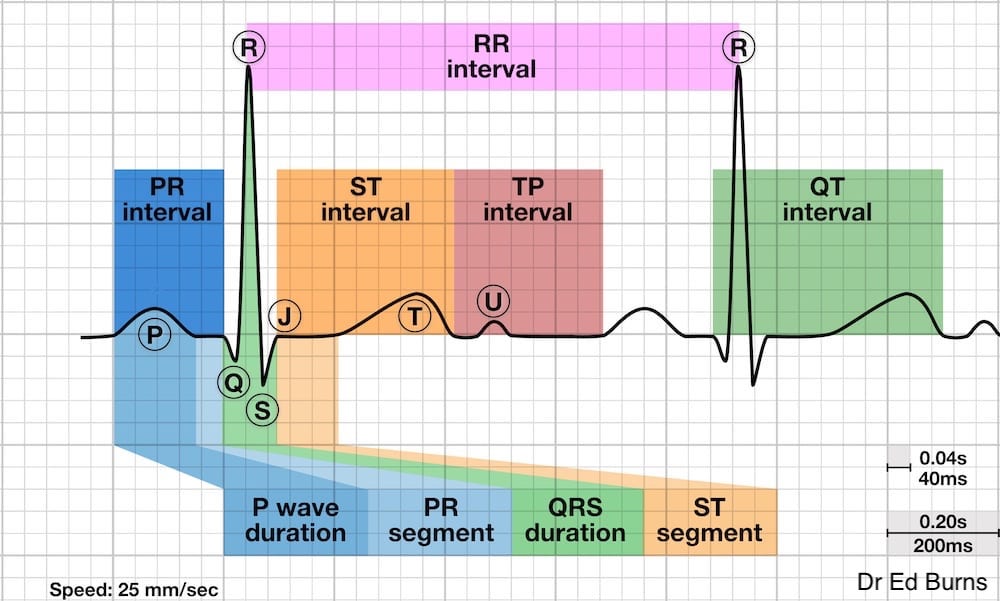
ECG, CBC, coags, renal function, VBG/lactate, Ammonia level, electrolytes, LFTs, type and cross, fibrinogen, CXR and EKG
Management:
First obtain bilateral IV access (large bore advised), monitors, supplemental oxygen. Wear personal protective equipment.
Airway:
This is one of the most difficult airways to management due to shock state, difficulty with visualization, rapid desaturation with sedative/paralytic, and extensive blood loss.
Use NG tube to decompress stomach (remove the ticking time bomb).
May use metoclopramide 10 mg or erythromycin 250 mg IV to assist in moving blood through GI tract
Place in Trendelenberg if vomiting (keep blood out of lungs).
Bleeding and Circulation:
Hemostatic Resuscitation: Do not rely on PT/PTT/INR to assess coagulation status. Consider use of TEG instead. May need to start MTP
Consider pRBCs if Hb <7 g/dL (goal of Hb between ≥7 g/dL (70 g/L) and <9 g/dL). If pt received >6 units of pRBCs in <3 hours check serum ionized calcium concentration (due to citrate binding of ionized calcium)
Platelets – if initial platelet count is < 50,000/microL
Prohemostatic products – consider fresh frozen plasma, PCC on case by case basis, cryoprecipitate targeting fibrinogen 150-200 mg/dL. Consider to use TXA 1g IV.
Target resuscitation end points of mentation, capillary refill, MAP, urine output.
Source Control: Emergency GI and IR consults.
May use erythromycin or metoclopramide to improve view for EGD.
Use octreotide 50 mcg IV bolus, 50 mcg/hr IV infusion (or vasopressin with nitroglycerin), which is associated with decreased products transfused.
Be ready with other devices: Sengstaken-Blakemore, Minnesota, Linton-Nachlas tubes.
https://www.youtube.com/watch?v=Yv4muh0hX7Y
Prevent and Treat Complications:
Infection associated with 25-65% of upper GI bleeds from varices (UTI, SBP, pneumonia):
Ceftriaxone 1 g IV or cefotaxime 2 g IV associated with NNT of 22 to prevent death and NNT of 4 to prevent infection.
Albumin also useful in patients meeting certain criteria (Cr 1.5, BUN > 30, bilirubin > 4)
Consider NG tube placement for stomach decompression (Whether placement of a nasogastric tube can help prevent aspiration has not been well studied)
Beware of renal failure and encephalopathy, which are further complications.
References: EMCrit, EMDoc, UpToDate