A 36-year-old man presents by ambulance following a motorcycle crash. He told the EMTs that he lost control and fell sideways, bracing his fall with his outstretched right hand. His R arm looks deformed but is neurovascularly intact. An xray is obtained.
What’s the name of this one again?!
Galeazzi fracture! Named after an Italian surgeon from Milan.
What is it? a fracture-dislocation of the distal third of the radius associated with dislocation-subluxation of the distal radial ulnar joint, or DRUJ.
Why do we care? With Galeazzi fractures, there is a high risk of malunion, loss of function, infection, and chronic pain in adult patients. For this reason, surgical management with internal fixation and possible open reduction is required. The repair should occur promptly, so the emergency physician or another clinician should contact the orthopedic consultant emergently to coordinate care.
What about in peds? Emergent orthopedic consultation is still required but interestingly, in children, some Galeazzi fractures are treated conservatively with closed reduction by an orthopedic surgeon. Disruption of the DRUJ can be subtle, so a high suspicion should be maintained when a patient presents with a fracture of the distal third of the radius.
Pearls of the Peal:
* Look for fracture-dislocation of the distal radius and ulna after a fall onto an outstretched arm. This injury can’t be missed: it requires immediate orthopedic involvement.
* Skin tenting associated with the Galeazzi fracture-dislocation puts the patient at risk for skin necrosis and conversion to an open fracture.
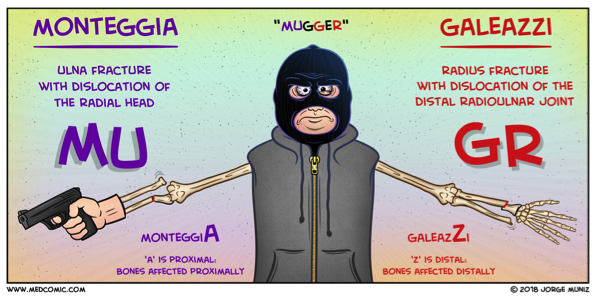
Wasn’t there some way to remember this compared to other one?? Why, yes! See below:
Sources:
Comic: Medcomic.com
Xray and clinical information: PEER IX