The pelvic ring consists of the sacrum and two innominate bones, which are made up of the pubis, ilium, and ischium. These bones are held together by strong ligaments to give the pelvis stability.
A pelvic ring fracture is a severe fracture with 2 breaks in the circular ring, leading to an unstable pelvis and a potentially unstable patient. Fractures that disrupt the pelvic ring predispose patients to bleeding given the large network of arterial and venous anastomoses. Patients who have an isolated pelvic fracture and are hypotensive carry a mortality of 15-40%. Most vascular injuries in the pelvis are venous (90%). While rare, arterial bleeds (10%) should be suspected when a pelvic binder is placed but the patient remains hemodynamically unstable. The retroperitoneal space can accumulate 4 liters of blood before venous tamponade occurs. Pelvic binders are useful in that they can help tamponade bleeding veins, decrease total pelvic volume, and prevent the shifting of bony fragments.
Other unstable pelvic fractures include lateral compression fractures, "open book" pelvic fractures, and vertical shear fractures. Lateral compression fractures occur when a lateral force vector (t-bone in an MVC) causes an anterior ring disruption and sacral fracture.
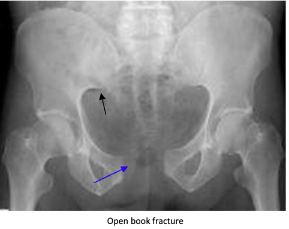
“Open book” fractures occur as a result of anteroposterior compression injury to the pelvis, commonly caused by high-speed trauma or elderly falls. There is a disruption to the pubic symphysis and the pelvis opens like a book. Diastasis of > 1 cm (blue arrow) can indicate instability. Disruption of the pubic symphysis, one of the strongest ligamentous structures in the human body, requires a lot of force and should be a red flag to look for other injuries to the head, spine, chest, or abdomen.
Vertical shear pelvic fractures are seen when one-half of the pelvis shifts upward as a result of a fracture of ipsilateral anterior and posterior pelvic ring fractures. They typically occur as a result of high-energy force applied in the axial direction (aka from the gas pedal to the femur and up to the pelvis). Patients may have an unstable pelvis and leg length discrepancy.
For all unstable fractures, you should appropriately resuscitate and stabilize the patient. Give blood as needed but avoid transfusing through lower limb access because it may drain into the retroperitoneal space. If there is a pelvic ring fracture, consider binding the pelvis. Your binder should lay over the greater trochanters and have enough force to close the pelvic ring (video:https://www.youtube.com/watch?v=tWLBZKeWEkg).