STEMI Equivalents
Hyperacute T Waves
in ≥ 2 contiguous leads
broad and asymmetric
concerning when upright T-wave in V1 > V6
also need to rule out hyperK
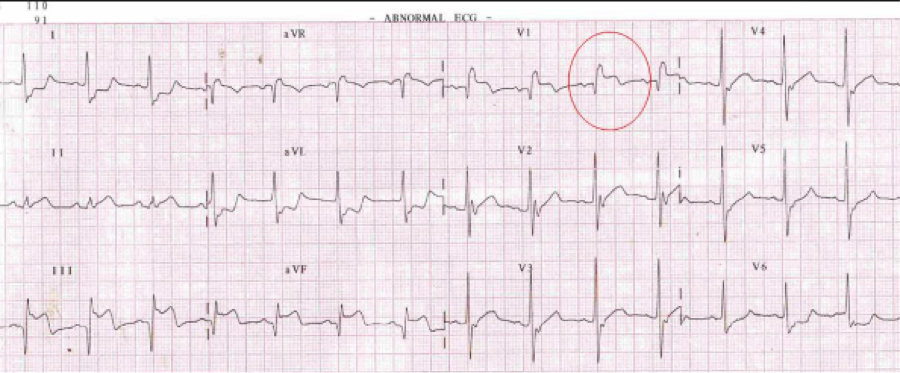
Wellen's Waves
Commonly in V/2/V3
Type A: biphasic T waves
Type B: more common; deep, symmetric T waves inversions
AVR
ST Elevation >1mm in AVR and/or V1 with diffuse depressions
LMCA occlusion, LAD occlusion, or triple vessel disease
Nonspecific, can also see this EKG with PE, aortic dissection, etc.
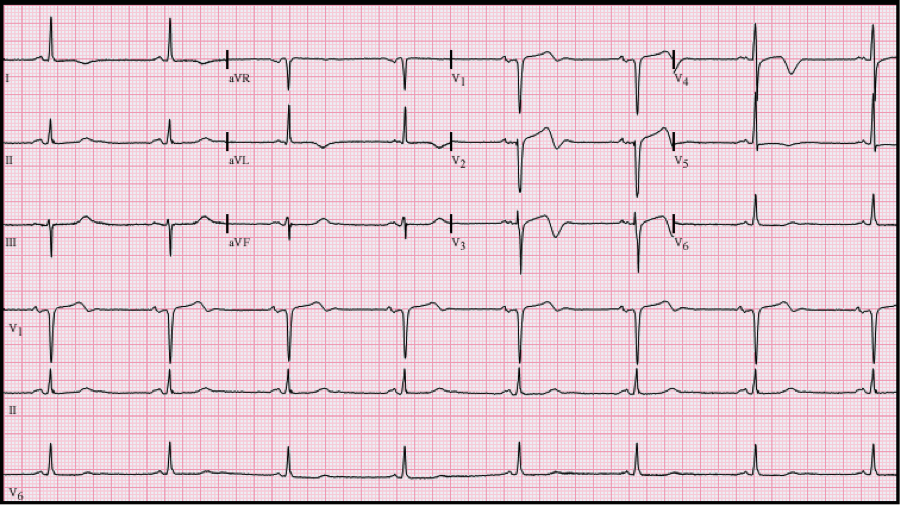
De Winter’s T Waves
ST depression with peaked T Waves
> 1 mm of upsloping ST depression and tall symmetric T-waves commonly in the precordial leads
Proximal LAD occlusion
Also consider:
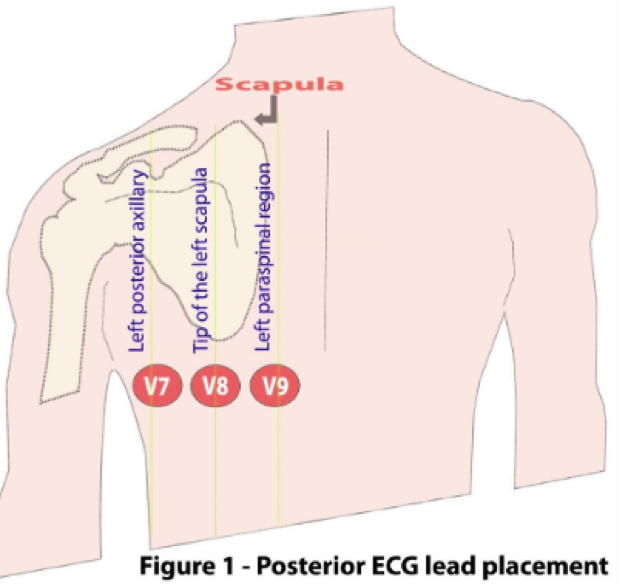
Posterior MI
ST depressions in V1-V3
Get posterior EKG with leads V7V8V9
STE ≥ 0.5 mm (≥ 1 mm in men < 40 years) in V7, V8, or V9
Left circumflex or RCA occlusion
Right Ventricular MI
should consider in your inferior STEMI pts
ST elevation in V1 (+/- V2 ST elevation OR depression)
ST elevation in lead III > lead II
Get a right sided EKG with leads V3V4V5
Can have elevations in these
RCA occlusion
AVL
T wave inversion in AVL
can also have hyperacute t waves in inferior leads
Think Inferior wall MI
https://rebelem.com/rebellion-in-em-2018-stemi-equivalents-by-tarlan-hedayati-md/
https://www.emra.org/emresident/article/stemi-equivalents/
https://wikem.org/wiki/ST-segment_elevation_myocardial_infarction