So, it's winter. Kids get sick. But really, 8-10 times a year is normal, so they're sick all the time! And they present to the ED with FEVER!!!!
What do you think about and what do you do with FEVER!?!?!?
- Fever = 38 degrees Celsius or 100.4 Fahrenheit
- Subjective fever per parents? Believe and work up/treat appropriately based on clinical presentation
- Determine exact onset and calculate fever duration (if since last night, it is only 1 day since <24 hours)
- Ask T-max
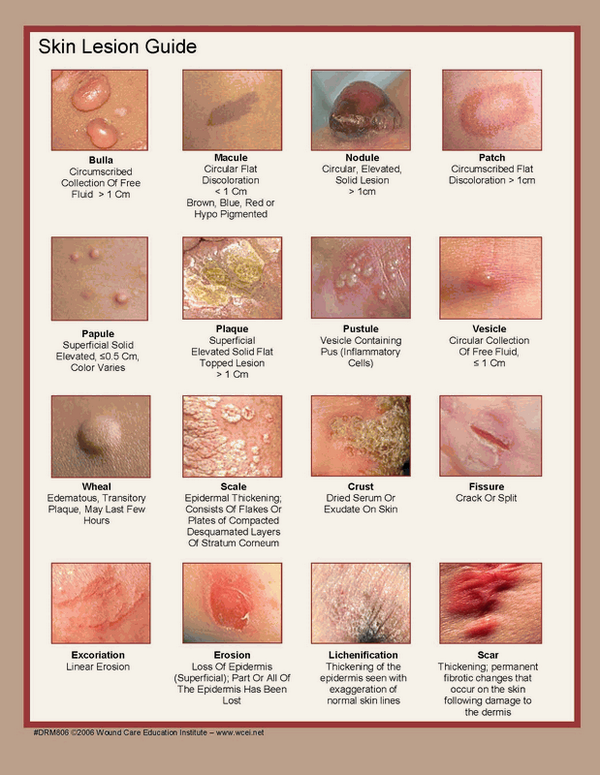
Thorough exams must include throat, ears, skin, oropharynx!
If suspect infectious etiology, treat with antipyretics:
Acetaminophen: 15 mg/kg every 4 hours, PRN
Ibuprofen (6 months and older): 10 mg/kg every 6 hours, PRN
The "alternating" approach of treating every 3 hours (Acetaminophen at 9, Ibuprofen at 12, Acet. at 3, etc) can help keep the kiddos' fever under control and keep them happy, hydrated, and hopefully home!
What to do!?
0-28 days infant:
Orders: CBC with differential, Blood Culture, BMP, UA with culture, LP with CSF gram stain/cell count/culture/possible viral culture. +/- HSV PCR. +/- stool culture if presenting with diarrhea. CXR
Pathogens: Group B Strep, E. Coli, Listeria. Consider HSV
Treatment: Ceftazidime or cefotaxime + Ampicillin (for Listeria). or Gentamycin + Ampicillin. +/- Acyclovir (< 21 days, seizures, rash, mom w/ lesions)
**No ceftriaxone: ceftriaxone displaced bilirubin and places patient at increased risk for Kernicterus
Dispo: Admit
29-60 days Infant:
Similar to above, but more experienced pediatric clinicians may use clinical judgement regarding LP. In general, most general EM physicians should practice more conservative management and pursue LP.
*Philadelphia/Rochester/Boston criteria for infants vary, hence the debate.*
Orders: CBC with differential, Blood Culture, BMP, UA with culture, LP with CSF gram stain/cell count/culture/possible viral culture. +/- HSV PCR. +/- stool culture if presenting with diarrhea. +/- CXR if respiratory symptoms.
Treatment: Ceftazidime or cefotaxime + Ampicillin or Ceftriaxone. Skin infection: +vancomycin
Dispo: often admit, but again, clinical judgement. If you diagnose a UTI in a well appearing, eating infant and labs are normal WBCs, no bandemia, normal CSF, consider 1 dose of ceftriaxone and 24 hour follow up (be mindful of patient's family's education, access to healthcare/the hospital, reliability, health literacy, etc.). Do what is best for the patient. See reference from CHOP for an example: https://www.chop.edu/clinical-pathway/febrile-infant-emergent-evaluation-clinical-pathway. Again - do what is best for the patient and appropriate for your level of pediatric training/experience.
Acute Otitis Media:
Bacteria: Strep pneumo (~80%), H. flu (especially if unvaccinated), Moraxella
Treatment: high dose Amoxicillin 90 mg/kg per day divided into 2 doses (to overcome strep pneumo's penicillin binding protein and H. flu's beta lactamase). If resistant, Augmentin (dose based off the amoxicillin)
Pneumonia:
Most common pathogens:
< 3 weeks: E. coli, Group B Strep, Listeria
> 3 weeks: Strep pneumonia
UTI: