This is probably bread and butter for us at Maimo and we are roughly familiar with how to manage it. Today, we take a deep dive into the classification and etiology of decompensated CHF to better understand the disease process. And then a short review on the basics of management just go through it systematically.
What is decompensated heart failure?
When something structural or functional happens to the heart, leading to inability to eject and/or accommodate blood within physiological levels.
Leads to a functional limitation
Requires immediate intervention
2 different scenarios:
1) New-onset acute CHF
No prior history or symptoms of CHF
Triggered by:
Acute MI
Hypertensive crisis
Rupture of chordae tendineae
Usually more prominent pulmonary congestion > systemic congestion
Usually normal blood volume
Treatment focused on treating underlying cause
High dose diuretics less helpful
2) Decompensated (chronic) CHF
Worsening of symptoms in existing CHF
Most commonly caused by:
Low treatment adherence - med noncompliance or poor diet (high salt)
Infection
PE
Tachy/bradyarrhythmias
Often new-onset afib
Factors indicating poor prognosis in DHF:
Pts with BUN > 90 and Cr > 2.75 on admission have a 21.9% risk of in-hospital mortality
Age (above 65 years)
Hyponatremia (sodium <130meq/L)
Impaired renal function
Anemia (hemoglobin <11g/dL)
Signs of peripheral hypoperfusion
Cachexia
Complete left bundle branch block
Atrial fibrillation
Restrictive pattern on Doppler
Persistent elevation of natriuretic peptides levels despite treatment
Persistent congestion
Persistent third heart sound
Sustained ventricular tachycardia or ventricular fibrillation
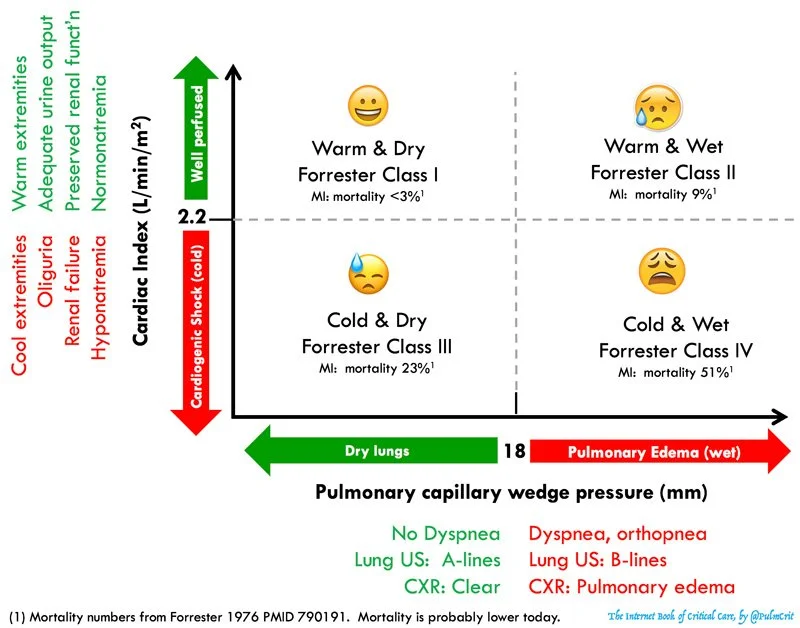
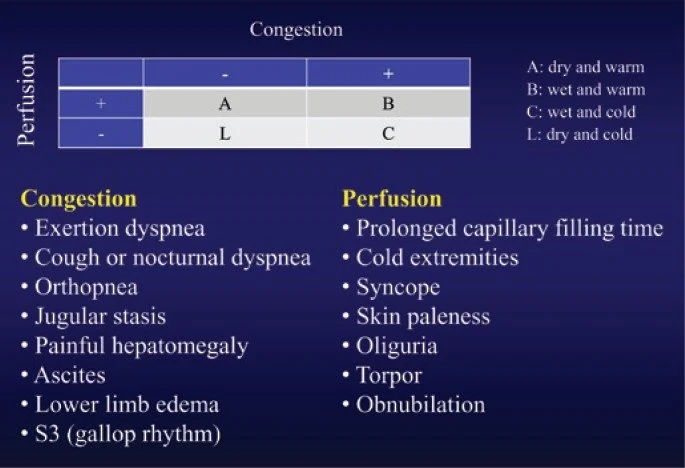
Classification system - Stevenson Classification (below)
Here’s another similar classification chart that’s more visually stimulating:
Forrester Classification (below)
Use to guide management
A (dry, warm) = compensated
B (wet, warm) = most common
Vasodilators and diuretics
Consider inotropes especially when SBP b/w 90-120
C (wet, cold) = worst prognosis
Ionotropes and diuretics
IV vasodilators if BP is being intensively monitored
L (dry, cold) = rare
Volume resuscitation +/- inotropes
Causes of CHF exacerbation
Tsuyuki et al, 180 pts
Most common primary cause: excessive salt intake (15%)
Noncardiac disorders (15%)
Inappropriate reductions in CHF therapy (9%)
Ghali et al, 101 pts at Cook County Hospital in Chicago
Lack of compliance with diet, drugs, or both (64.4%)
Uncontrolled HTN (43.6%)
Cardiac arrhythmias (28.7%)
Opasich et al, 161 pts referred to CHF service at Italian hospital
Arrhythmias (24%)
Infection (23%)
Poor compliance (15%)
Angina (14%)
My takeaway: there is wide variability in the causes of DHF and limited studies out there about the various causes. Given that poor medication / diet compliance is often at the top of the list, it seems like good patient education may go a long way in preventing CHF exacerbation. Consider taking the time to really get at why your patient is in CHF exacerbation. Do they not understand how often they’re supposed to take their diuretic? Are they in denial about junk food intake?
You MUST understand the classification of your patient’s CHF in order to manage them appropriately. It’s not always cookie cutter diuretics.
I also decided to touch on basics of CHF management because I thought this was a nice review by emcrit.
1. Treat the lungs
BIPAP - reduce preload and afterload (like ACEI)
Intubation - cardiogenic shock
Drain large pleural effusions if causing respiratory distress
Inhaled pulmonary bronchodilator - epoprostanol or NO
2. Optimize MAP - reduce afterload if pt can tolerate
High dose nitroglycerin - up to 200-250 mcg/min
Transition to oral once stabilized - ACEI, ARB, hydralazine + isosorbide dinitrate
Manage hypotension with pressor - NOREPINEPHRINE IS KING
EPI is reasonable if reduced EF, hypotensive, with poor cardiac output
AVOID dopamine - evidence of harm compared to NE in SOAP-II trial
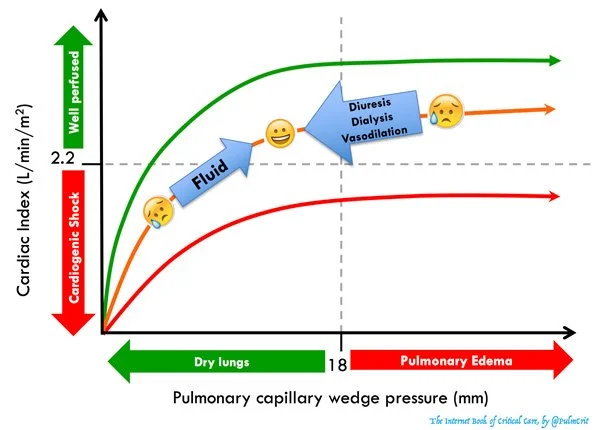
3. Optimize volume status
Fluids?
End organ perfusion (AKI)
NO evidence of pulmonary congestion (no B lines on US)
Appears truly hypovolemic (no systemic congestion)
Give small boluses at a time and reassess
Diuresis?
SIgnificant pulmonary or systemic congestion
Overall appears hypervolemic
4. Inotrope for HFrEF
Very temporary improvement in hemodynamics and actually associated with worse outcomes in some studies
Inotropes should ONLY be used if:
Hypoperfusion with low-normal BP (like AKI with poor UO despite above interventions)
Refractory cardiogenic pulmonary edema (like if the interventions above don’t work and you still need to reduce pulmonary congestion)
Dobutamine?
Shorter half life, more titratable than milrinone
Preferred for immediate stabilization of very ill patient, someone with marked pulmonary edema on the verge of intubation
Milrionone?
More effective vasodilation than dobutamine
Renally excreted so tricky to titrate dose in renal failure - half life 2.3 hours in normal kidneys
DIgoxin?
The only positive inotrope that doesn’t correlate with increased mortality
Consider for patients with long standing afib and systolic HF
Not front line
5. Treat underlying cause
New onset tachyarrhythmia - convert to sinus. Beware slowing HR if it isn’t high already
Cardiogenic shock 2/2 MI - ASA, antiplatelet, anticoagulation
Revascularization is essential!!! Valuable even if delayed.
Thrombolysis works poorly
THINGS TO AVOID:
Anything nephrotoxic - NSAIDs, ACE/ARB
DO NOT suppress sinus tach since this is usually compensatory and keeping the patient alive
Avoid diltiazem in afib with DHF
Do NOT treat mild stable hypoNa with hypertonic or salt tablets
Fluid and sodium restriction actually haven’t shown benefit in RCTs once they are in decompensated HF
BEWARE BETA BLOCKERS - don’t start them in decompensated heart failure
Great for chronic compensated HF
Negative inotrope could impair cardiac function
Controversial if BB should be continued in patients who are already taking them -- in general should be held in cardiogenic shock
References
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/649270
jamanetwork.com
Background Few studies have prospectively and systematically explored the factors that acutely precipitate exacerbation of congestive heart failure (CHF) in patients with left ventricular dysfunction. Knowledge of such factors is important in designing measures to prevent deterioration of...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4878602/
www.ncbi.nlm.nih.gov
Heart failure is a disease with high incidence and prevalence in the population. The costs with hospitalization for decompensated heart failure reach approximately 60% of the total cost with heart failure treatment, and mortality during hospitalization ...
https://emcrit.org/ibcc/chf/#hemodynamic_evaluation_&_risk_stratification
Forrester classification
Forrester classification - management
Stevenson classification