Let’s talk about FOOSH (say that 3 times fast) injuries. That’s falling on an outstretched hand, you know so you don’t eat dirt. Falling this way can result in a number of upper extremity injuries and we will highlight some of the common fracture patterns.
Distal radius fractures
Colles fractures – think old lady with osteoporosis or high impact trauma.
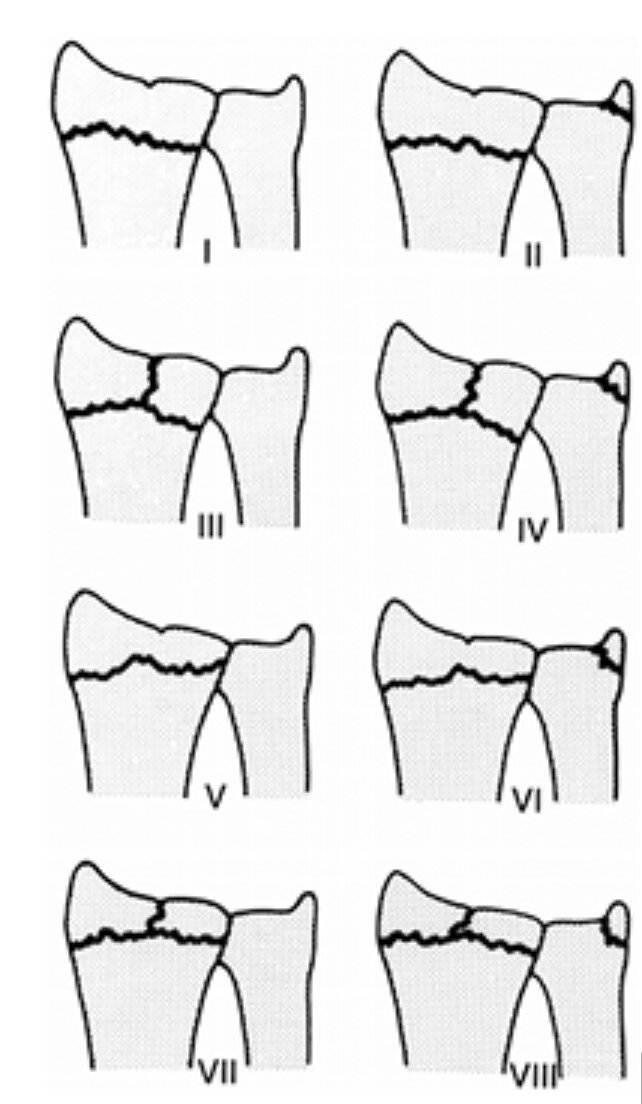
There’s a classification called the Frykman classification system. It’s really just 4 main types in the left column and the right column adds on an ulnar styloid fracture
Most treated with closed reduction and short arm cast.
Smith fractures – it’s much less common, think of it as a reverse Colles fracture. You get it by falling onto a flexed wrist or a blow to the back of the wrist. So you’re going to have volar angulation. Compare that to the Colles.
Most are also treated with closed reduction and short arm cast.
Forearm fractures
Galeazzi fractures – children usually, especially ages 9-12. FOOSH with elbow in flexion. It is a radial shaft fracture + dislocation of the distal radioulnar joint.
Usually unstable and needs OR.
Monteggia fractures – Children usually as well especially age 4-10. Ulnar shaft fracture + dislocation of radial head. Cast or ORIF depending on the type.
A common mnemonic is MUGR (or GRUM)
Monteggia involves fracture of the ulna with proximal radial dislocation
Galeazzi involves fracture of the radius with distal radioulnar dislocation
Carpal bone fractures
Scaphoid fractures – most common, pain in the anatomical snuffbox. Risk of avascular necrosis. Thumb spica splint + ortho f/u if there is pain even without obvious fracture on x-ray. If there is an apparent fracture on imaging, get an ortho consult because there is a risk of non-union or malunion and they may offer surgery.