Clinical Scenario:
A 30-year-old woman presents with headache, fever, and decreased vision in her right eye over the past 24 hours. Examination reveals exophthalmos of the right eye and no pupillary reflex and a clear anterior chamber. When asked, she denies weakness and numbness.
What is the most likely diagnosis?
Last week we talked about cerebral venous sinus thrombosis (CVST), today let’s talk about cavernous sinus thrombosis (CST), or the infected subset of cerebral venous sinus thrombosis.
What is it?
Cavernous sinus thrombosis (CST) is a rare condition, defined as a septic thrombophlebitis of the cavernous sinus. It is caused by a bacterial infection that typically originates in the face, sinuses, ears, or orbits. Most infectious etiologies in cavernous sinus thrombosis are from Staphylococcus or Streptococcus species.
The two cavernous sinuses are located on both sides of the sella turcica. Important structures are located in, or run through, the cavernous sinus, including the pituitary gland, cranial nerves III, IV, V and VI, and the internal carotid arteries (ICA).
It causes significant morbidity and the mortality rate is at 20-30%.
Risk Factors
Sphenoid and ethmoid sinusitis are the most common causes of CST.
Other risk factors include dental infections, facial cutaneous infections, otitis media, maxillofacial surgery, and trauma.
Presentation
Most patients will have fever, headache, and vision changes/ocular complaints (proptosis, periorbital edema and/or chemosis).
Most will also have external ophthalmoplegia, due to venous congestion of orbital tissues, extra-ocular muscle inflammation and/or inflammation of cranial nerves III, IV and VI.
Other symptoms include eyelid erythema, autonomic dysfunction, sensory changes in the ophthalmic and maxillary trigeminal nerve distributions, pupillary abnormalities, and papilledema.
Vision loss is rare as the orbital nerve lies outside the cavernous sinus.
CST commonly spreads from one eye to both within 24 to 48 hours.
Evaluation
Blood cultures, CBC, and coagulation studies (PT and PTT) should be ordered, as well as CT of the head and orbits with contrast.
Treatment
Parenteral antibiotic treatment should be started with gram-positive coverage (nafcillin plus a third-generation cephalosporin or vancomycin if concerned for MRSA). The patient should be admitted with neurology and ophthalmology consultations
Anticoagulation and steroids, remain controversial.
Steroids may confer improved cranial nerve function.
Anticoagulation may confer a risk of systemic and intracranial bleeding and may result in dissemination of septic emboli. Consider anticoagulation only if there is no evidence of severe bleeding risk or current hemorrhage.
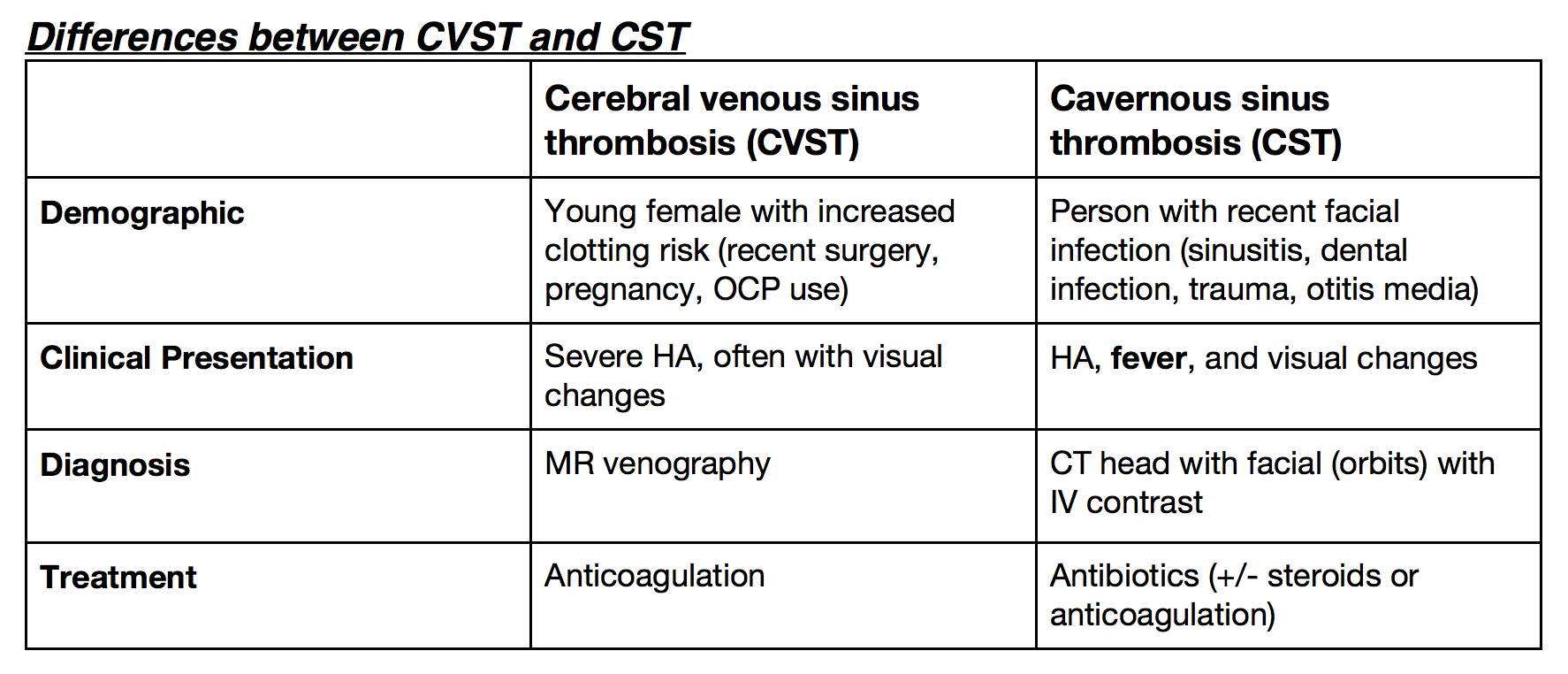
Differences between CVST and CST