I’ve maybe had to think about this twice during residency and both times was like ??? so I figured I should at least learn a little about it.
Although slowly dying out in terms of popularity, some providers STILL put their patients on warfarin. One of the last conditions where warfarin is indicated over a DOAC is in the setting of a mechanical valve, which can be a clue into the patient’s past medical history if you see it on their medication list (or that their PCP is old school). And even this may change as data on DOAC’s continues to evolve. There are multiple reasons why warfarin is a very annoying drug to work with.
1) Narrow therapeutic window – for most indications the target INR is between 2-3
2) Variable dose response
3) Multiple drug-diet and drug-drug interactions
4) Requiring bridging therapy
The main benefit of warfarin is that in the event of bleeding or hemorrhage, there are easy and effective reversal agents.
So, what happens if you shotgun labs on a patient (as one does) and their INR returns at a higher level? Like 4? 7? 10?? It depends on the scenario.
Significant or Life-Threatening Bleeding – very obvious, no thought involved. Obviously do not wait for confirmatory testing before treating.
- Stop warfarin
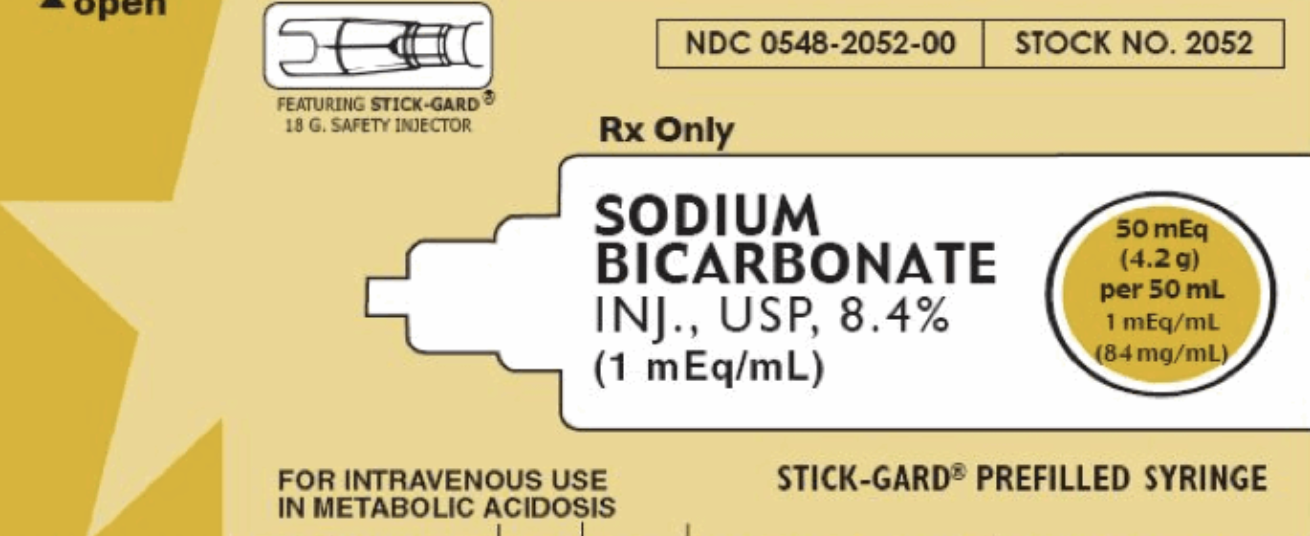
- Give Vitamin K 10mg IV over 20-60min. Some considerations…
o Vitamin K works by helping the body produce more coagulation factors (no, I won’t go over the mechanism). This takes more than a few hours and does not help immediately
o If started on vitamin K the patient will usually be refractory to warfarin for some time, but this is less of a problem as a different (and likely better) anticoagulant can be started in the interim
- 4-factor prothrombin complex concentrate (PCC) – Kcentra (what we have at Maimonides). I think this will end up institution specific, but we do…
o Fixed approach – does not depend on INR. After a lovely discussion with pharmacy, studies appear to show that it is just as effective but lowers cost as overall doses are lower. Preferred if you have a choice.
§ GI/ENT/life-threatening hemorrhage – 1500 IU
§ ICH – 2000 IU
o INR-based approach – start off with 1500 IU empirically then add SUPPLEMENTAL dose…
§ INR 2-4: total 25 IU/kg (max 2500)
§ INR 4-6: total 35 IU/kg (max 3500)
§ INR > 6: total 50 IU/kg (max 5000)
- If no Kcentra, consider FFP (but it honestly sounds like you should never really consider FFP). Per UpToDate…
o 2U FFP. Check INR 15 min after infusion, if >1.5 give another 2IU. Repeat until INR < 1.5.
o Consider Lasix if infusing large amounts
Luckily, the order set reflects this at Maimonides, and we don’t have to think about it here.
Not really a debate anymore, but Kcentra vs FFP? Kcentra…
- Is more rapid and effective at correcting INR - ~30 min
- Can be infused faster with less volume less likely leading to fluid overload
- Shorter preparation time
- Does not require blood-type matching
- FFP is cheaper though…. +1
For Urgent/Emergent procedures
- Treat as above in discussion with surgeon or proceduralist
- If it can wait, don’t need to treat as aggressively
Minor Bleeding (like epistaxis) – very complicated, decided by many factors and heavily decided by physician judgement. Some things to consider
- Extent of bleeding and risk of progression
- Previous bleeding history
- Comorbidities (CKD, HTN)
- Concomitant anti-platelet therapy
- INR level
- Thromboembolic risk of the patient (prosthetic valve, atrial fibrillation, history stroke/DVT/PE, etc.)
- Therapy will range from holding warfarin, giving vitamin K, and treating as above
Now on to why I actually decided to make this POTD.
Asymptomatic Elevated INR – based on INR
- INR > 10: oral vitamin K 2.5-5mg response in 24-48 hours
o Hold warfarin
o No role for Kcentra or FFP
o INR should be checked daily or every other day, repeat oral vitamin K as needed
- INR 4.5-10
o Hold warfarin (1-2 doses)
o Can consider low dose oral vitamin K – 1 - 2.5mg. Again, consider SEVERAL factors
§ Risk of bleeding – older age, prior bleeding, higher INR consider oral vitamin K
§ Risk of thrombosis
- INR <4.5
o Hold next dose of warfarin (or reduce dose, this is generally on the PCP though)
o Needs more frequent INR checks in the immediate future
Does anyone NEED to be admitted for management of supratherapeutic INR? Likely not. Fortunately, or unfortunately, depends on our clinical judgement. Off the top of my head…
- Consider calling PCP to ensure follow-up / PCP comfort
- Consider risk of bleeding vs. risk thrombosis
- Patient ability to follow up
- The thousand other things we think about when deciding whether to admit or discharge patients
What about an elevated INR in a liver patient?
- Do not treat like warfarin-induced elevated INR
- Patients are usually at baseline PRO-THROMBOTIC from low levels of protein C and S (anticoagulation factors)
- Nothing to really do for elevated INR in the cirrhotic patient – per UptoDate appears that most attempts to correct lead to adverse events (thrombosis, etc.)
TL;DR
- Ensure proper patient follow-up for cases of asymptomatic supratherapeutic INR
- INR > 10 – hold warfarin, consider 2.5 – 5mg oral vitamin K
- INR 4.5-10 – hold warfarin, consider 1 – 2.5mg oral vitamin K
- INR < 4.5 – hold a single dose and recheck INR (not in ED)
https://www.nuemblog.com/blog/supratherapeutic-inr
http://www.emdocs.net/em-cases-liver-emergencies/